EFFECTIVE JANUARY 1, 2024
Employee
Benefit Summary
MEDICAL, DENTAL,
VISION, DRUG, FSA,
LIFE INSURANCE,
403(b ) & 457(b ) ,
AND RETIREMENT
BENEFITS
Employee and Reree Service Center ¡ 45 W. Gude Drive, Suite 1200, Rockville, MD 20850
301-517-8100 ¡ www.montgomeryschoolsmd.org/departments/ersc
2024
Benefits Plan Highlights for 2024
¡ There are no changes to MCPS-offered medical, prescription,
dental, or vision plans for 2024.
VISION
We inspire learning by
providing the greatest
public education to each
and every student.
MISSION
Every student will have
the academic, creative
problem solving, and
social emotional skills
to be successful in
college and career.
CORE PURPOSE
Prepare all students to
thrive in their future.
CORE VALUES
Learning
Relationships
Respect
Excellence
Equity
Board of Education
Ms. Karla Silvestre
President
Mrs. Shebra L. Evans
Vice President
Ms. Lynne Harris
Ms. Grace Rivera-Oven
Mrs. Rebecca K. Smondrowski
Ms. Brenda Wolff
Ms. Julie Yang
Mr. Sami Saeed
Student Member
Montgomery County Public Schools (MCPS)
Administration
Monifa B. McKnight, Ed.D.
Superintendent of Schools
Mr. M. Brian Hull
Chief Operating Officer
Patrick K. Murphy, Ed.D.
Deputy Superintendent
Mr. Brian S. Stockton
Chief of Staff
Mrs. Stephanie P. Williams
General Counsel
Ms. Elba M. Garcia
Senior Community Advisor
Dr. Patricia E. Kapunan
School System Medical Officer
850 Hungerford Drive
Rockville, Maryland 20850
www.montgomeryschoolsmd.org
MCPS NONDISCRIMINATION STATEMENT
Montgomery County Public Schools (MCPS) prohibits illegal discrimination based on race, ethnicity, color, ancestry, national origin,
nationality, religion, immigration status, sex, gender, gender identity, gender expression, sexual orientation, family structure/
parental status, marital status, age, ability (cognitive, social/emotional, and physical), poverty and socioeconomic status,
language, or other legally or constitutionally protected attributes or affiliations. Discrimination undermines our community’s
long-standing efforts to create, foster, and promote equity, inclusion, and acceptance for all. The Board prohibits the use of
language and/or the display of images and symbols that promote hate and can be reasonably expected to cause substantial
disruption to school or district operations or activities. For more information, please review Montgomery County Board of
Education Policy ACA, Nondiscrimination, Equity, and Cultural Proficiency. This Policy affirms the Board’s belief that each and every
student matters, and in particular, that educational outcomes should never be predictable by any individual’s actual or perceived
personal characteristics. The Policy also recognizes that equity requires proactive steps to identify and redress implicit biases,
practices that have an unjustified disparate impact, and structural and institutional barriers that impede equality of educational
or employment opportunities. MCPS also provides equal access to the Boy/Girl Scouts and other designated youth groups.**
For inquiries or complaints about discrimination against
MCPS students*
For inquiries or complaints about discrimination against
MCPS staff*
Director of Student Welfare and Compliance
Office of District Operations
Student Welfare and Compliance
850 Hungerford Drive, Room 55, Rockville, MD 20850
240-740-3215
SWC@mcpsmd.org
Human Resource Compliance Officer
Office of Human Resources and Development
Department of Compliance and Investigations
45 West Gude Drive, Suite 2500, Rockville, MD 20850
240-740-2888
For student requests for accommodations under
Section 504 of the Rehabilitation Act of 1973
For staff requests for accommodations under
the Americans with Disabilities Act
Section 504 Coordinator
Office of School Support and Well-being
Office of Well-being, Learning and Achievement
850 Hungerford Drive, Room 257, Rockville, MD 20850
240-740-5630
504@mcpsmd.org
ADA Compliance Coordinator
Office of Human Resources and Development
Department of Compliance and Investigations
45 West Gude Drive, Suite 2500, Rockville, MD 20850
240-740-2888
For inquiries or complaints about sex discrimination under Title IX, including sexual harassment, against students or staff*
Title IX Coordinator
Office of District Operations
Student Welfare and Compliance
850 Hungerford Drive, Room 55, Rockville, MD 20850
240-740-3215
TitleI[email protected]
* Discrimination complaints may be filed with other agencies, such as the following: U.S. Equal Employment Opportunity Commission (EEOC),
Baltimore Field Office, GH Fallon Federal Building, 31 Hopkins Plaza, Suite 1432, Baltimore, MD 21201, 1-800-669-4000, 1-800-669-
6820 (TTY); Maryland Commission on Civil Rights (MCCR), William Donald Schaefer Tower, 6 Saint Paul Street, Suite 900, Baltimore, MD
21202, 410-767-8600, 1-800-637-6247, mccr@maryland.gov; or U.S. Department of Education, Office for Civil Rights (OCR), The Wanamaker
Building, 100 Penn Square East, Suite 515, Philadelphia, PA 19107, 1-800-421-3481, 1-800-877-8339 (TDD), OCR@ed.gov, or www2.ed.gov/
about/offices/list/ocr/complaintintro.html.
**This notification complies with the federal Elementary and Secondary Education Act, as amended.
This document is available, upon request, in languages other than English and in an alternate format under the Americans with Disabilities
Act, by contacting the MCPS Office of Communications at 240-740-2837, 1-800-735-2258 (Maryland Relay), or PIO@mcpsmd.org.
Individuals who need sign language interpretation or cued speech transliteration may contact the MCPS Office of Interpreting Services
at 240-740-1800, 301-637-2958 (VP) mcpsinterpretingservices@mcpsmd.org, or MCPSInterpretingServices@mcpsmd.org.
July 2023
2024
Montgomery County Public Schools
2024 Employee Benefit Summary for Active Employees
Montgomery County Public Schools (MCPS) provides a comprehensive benefit plan for employees,
retirees, and their eligible dependents. As an eligible MCPS employee, you have a variety of benefit
options from which to choose, including benefits to protect your health, your income, and your future.
The Employee Benefit Summary provides an overview of the benefits available to eligible active
employees, effective January 1, 2024. This summary includes information about eligibility for MCPS
benefits, a list of benefit costs, opportunities to reduce benefit costs through the Wellness Initiatives
program, and important contact information. It also includes instructions for accessing the online Benefits
Enrollment System (BES) during Open Enrollment, for new employees enrolling in benefits for the first
time and for employee experiencing a qualifying life event during the plan year.
Keep in mind that this is a summary of the MCPS benefit plan and is intended to help you understand and
properly enroll in the plan. Full benefit plan details are available on the Employee and Retiree Service
Center (ERSC) website at www.montgomeryschoolsmd.org/departments/ersc. The website includes
summary plan and evidence of coverage documents, along with links to provider websites.
ERSC staff members are available to assist you in person Monday through Friday from 8:00 a.m.–4:30
p.m., by telephone Monday–Friday from 8:00 a.m.–4:15 p.m., and via email. Our address, telephone
number, and email address are below:
Montgomery County Public Schools
Employee and Retiree Service Center
45 West Gude Drive, Suite 1200
Rockville, Maryland 20850
301-517-8100
Important Notice
You are not enrolled automatically in the MCPS employee benefit plan. New employees must enroll online within 60 days following
employment or wait for a future Employee Benefits Open Enrollment, typically held for four weeks beginning in early October, with
coverage effective January 1 of the following year. To enroll online, new employees must log in to the Benefits Enrollment System
(BES) by visiting the Employee Self Service (ESS) web page at:
www.montgomeryschoolsmd.org/departments/ersc/employees/employee-self-service/
From there, click the Benefits enrollment for new employees link, log in with your Outlook username and password, and follow
the onscreen instructions.
During Open Enrollment, employees visit the ESS web page and click the Open Enrollment link to log in to the BES and make
changes to their benefits. Outside of Open Enrollment, employees who experience a qualifying life event or return from long-term
leave must visit ESS and click the Benefits enrollment/changes due to a qualifying life event link to log in to BES and re-enroll in
or make changes to their benefits.
2024
Table of Contents
About Your Benefits ................................................................................................................... 1
Who is Eligible ............................................................................................................................................. 1
Eligible Dependents .............................................................................................................................. 1
Disabled Dependents ............................................................................................................................ 1
When Benefits Coverage Begins .................................................................................................................. 2
Special Rule for Newly Hired 10-Month Employees ........................................................................... 2
Special Rule for 10-Month Employees Who Terminate Employment or Retire .................................. 2
Enrolling New Dependents ........................................................................................................................... 2
Changes in or Cancellation of Coverage ....................................................................................................... 3
Loss of Non-MCPS Coverage .............................................................................................................. 4
Paying for Coverage ..................................................................................................................................... 4
When Benefits Coverage Ends ..................................................................................................................... 4
Special Rule for 10-month Employees ................................................................................................. 5
Continuation of Benefits (COBRA) .............................................................................................................. 5
Insurance Coverage While on Leave ............................................................................................................ 5
Out-of-Area Coverage .................................................................................................................................. 6
Coordination of Benefits ............................................................................................................................... 6
Birthday Rule ........................................................................................................................................ 6
Enrollment in Medicare ................................................................................................................................ 7
Enrollment Basics ....................................................................................................................... 8
Using the Online Benefits Enrollment System (BES) .................................................................................. 8
Submitting Supporting Documentation ........................................................................................................ 8
Your Benefits at a Glance .......................................................................................................... 9
Wellness Initiatives ................................................................................................................... 10
Biometric Health Screenings ...................................................................................................................... 10
Health Risk Assessments ............................................................................................................................ 10
Medical Coverage ..................................................................................................................... 10
Point-of-Service Plan .................................................................................................................................. 11
Cigna Open Access Plus .................................................................................................................... 11
Health Maintenance Organizations ..................................................................................................... 12
Cigna Open Access Plus In-Network ................................................................................................. 11
Kaiser Permanente HMO .................................................................................................................... 12
Preventive Care Services ............................................................................................................................ 12
Other Benefit Plan Coverage ................................................................................................... 18
Dental Coverage ........................................................................................................................ 18
CareFirst Preferred Dental Plan (PPO) ....................................................................................................... 18
Aetna Dental Maintenance Organization (DMO) ....................................................................................... 19
2024
Kaiser Permanente Dental Plan................................................................................................................... 19
Vision Coverage ........................................................................................................................ 21
Davis Vision Plan ....................................................................................................................................... 21
Kaiser Vision Plan ...................................................................................................................................... 22
Prescription Drug Coverage .................................................................................................... 22
CVS/Caremark Prescription Plan................................................................................................................ 22
Kaiser Permanente Prescription Plan .......................................................................................................... 26
Life Insurance ............................................................................................................................ 27
Employee Life Insurance ............................................................................................................................ 27
Basic Employee Term Life Insurance ................................................................................................. 27
Optional Employee Term Life Insurance............................................................................................ 27
Dependent Term Life Insurance ................................................................................................................. 28
Basic Dependent Term Life Insurance ............................................................................................... 28
Optional Dependent Term Life Insurance .......................................................................................... 28
Flexible Spending Accounts .................................................................................................... 28
403(b) Tax Sheltered Savings and 457(b) Deferred Compensation Plans .......................... 30
Applying for Distribution of Funds from 403(b) and/or 457(b) Accounts After Retirement ............. 31
Well Aware: Employee Wellness Program ............................................................................... 31
Retirement Benefits .................................................................................................................. 32
Social Security ............................................................................................................................................ 32
Pension Plans .............................................................................................................................................. 32
Postretirement Health Benefits ................................................................................................................... 32
Wellness Initiatives in Retirement .............................................................................................................. 32
Employee Benefit Rate Charts ................................................................................................. 33
2024
EMPLOYEE BENEFIT SUMMARY
1
About Your Benefits
WHO IS ELIGIBLE
You are eligible to enroll in the employee
benefit plan if you are a permanent MCPS
employee regularly scheduled to work 20 hours
or more per week. If your spouse has health
coverage through the MCPS employee benefit
plan and you are a covered dependent, you may
not enroll for coverage as an individual under
the MCPS employee benefit plan.
Eligible Dependents
You may choose to cover your eligible dependents
under the MCPS employee benefit plan. Eligible
covered dependents must be enrolled in the same
benefits plan in which you are enrolled.
Eligible dependents include your—
spouse, and
eligible children who meet the following age
requirements:
o until the end of the month in which they
turn 26 for medical and prescription
coverage
o until the end of the month in which they
turn 24 for dental and vision coverage
o until September 30 following their 23rd
birthday for life insurance coverage
The documentation you submit to show
eligibility of a spouse or child(ren) must include
but is not limited to the following:
Spouse:
Social Security card and
valid marriage certificate or current joint tax
return (signed by both parties or a copy of
the confirmation of electronic submission)
Newborn or Biological Children:
Social Security card and
valid birth certificate or valid birth
registration
Stepchildren:
Social Security number and
valid birth certificate or valid birth
registration and
shared or joint custody agreement (court
validated) up to age 18
Adopted Children, Foster Children, Children in
Guardianship or Custodial Relationships:
Social Security number and one of the
following:
o adoption documents (court validated)
o guardianship or custody documents
(court validated)
o foster child documents (county, state, or
court validated)
Disabled Dependents
Any disabled dependent child remains eligible
for medical and prescription coverage until the
end of the month in which he/she turns 26. A
disabled dependent remains eligible for dental,
and vision coverage until the end of the month in
which he/she turns 24. Disabled dependents
remain eligible for life insurance coverage until
September 30 following his/her 23rd birthday.
However, your disabled dependent child(ren)’s
coverage may be continued beyond these age
limits if—
he or she is permanently incapable of self-
support because of intellectual disability or
physical disability, or he/she became
disabled, and
the disability occurred before he or she
reached age 19.
It is your responsibility to notify MCPS of the
child’s incapacity and dependency to be
considered for continuous benefits coverage. If
MCPS is not notified prior to—
the dependent’s 26
th
birthday, medical and
prescription benefits will be cancelled;
the dependent’s 24
th
birthday, dental and
vision coverage will be cancelled; and

2024
EMPLOYEE BENEFIT SUMMARY
2
September 30 following the dependent’s 23
rd
birthday, life insurance will be cancelled.
Unless otherwise terminated in accordance with
the plan terms, coverage will continue as long as
the disabled child is incapacitated and
dependent. You will be asked to provide the plan
administrator with proof that the child’s
incapacity and dependency existed prior to age
19. Before the plan administrator agrees to the
extension of coverage, the plan administrator
may require that a physician chosen by your
health plan examines the child.
The plan
administrator may ask for ongoing proof that the
child continues to be disabled. If you do not
provide proof that the child’s incapacity and
dependency existed prior to age 19, as described
above, coverage for that child will end at the end
of the month in which he/she turns age 26 for
medical and prescription coverage, at the end of
the month in which he/she turns age 24 for
dental and vision coverage, and on September
30 following his/her 23
rd
birthday for life
insurance.
If you change your medical plan, you will be
required to submit new medical documentation
to the new health plan provider for review.
Coverage ends if you predecease your disabled
dependent, except as provided under federal
Consolidated Omnibus Budget Reconciliation
Act (COBRA) legislation.
WHEN BENEFITS COVERAGE
BEGINS
New employees must enroll in benefits via the
online Benefits Enrollment System (BES) within
60 days of initial employment or wait until a
future Open Enrollment to enroll online. (See
Enrollment Basics in this booklet for benefits
enrollment instructions.) Coverage begins on the
first day of the month following the month that
you enroll, provided you submit your online
enrollment by the 20th day of the month.
If you enroll online after the 20
th
day of the
month, your benefits coverage begins on the first
day of the second month. For example, let’s
assume you are hired on December 23. Refer to
the chart below to see when your coverage
would begin:
If you submit your
online enrollment:
Your coverage will
begin on:
On or before January 20
February 1
Between January 21 and
February 20
March 1
On February 21
April 1
Special Rule for Newly Hired
10-Month Employees
If you are a 10-month employee reporting at the
beginning of a school year, your coverage will
begin October 1 if you enroll by September 20.
If you enroll from September 21 to October 20,
your coverage will begin November 1. You must
enroll within 60 days of initial employment.
Special Rule for 10-Month
Employees who Terminate
Employment or Retire
A 10-month employee who terminates
employment or retires prior to their last duty day
will be issued a refund for any pre-paid health
insurance deductions (medical, dental, vision,
prescription).
A 10-month employee who terminates
employment as of their last duty day or retires
effective July 1, August 1, or September 1 will
maintain their health benefits through September
30. This is the date through which their benefits
have been prepaid.
ENROLLING NEW DEPENDENTS
Your new dependents are not covered or
enrolled automatically under the benefit plan—
you must take action to enroll new dependents in
your plan. You may enroll a new eligible
dependent in your benefit plan during Open
Enrollment or when you experience a qualifying
life event.
2024
EMPLOYEE BENEFIT SUMMARY
3
Please note that you must enroll your new
dependent through ERSC, not through the
benefit plan provider.
When you enroll a dependent in your plan,
whether as a new employee, during Open
Enrollment, or due to a qualifying life event, you
are required to use the BES. (See Enrollment
Basics in this booklet for benefits enrollment
instructions.) You will be required to provide
supporting documentation.
Refer to the chart below for information about
enrolling an eligible dependent if you experience
a qualifying life event. It includes important
deadlines and documentation you are required to
submit. Note: All documentation must be
translated to English prior to submitting it to
ERSC.
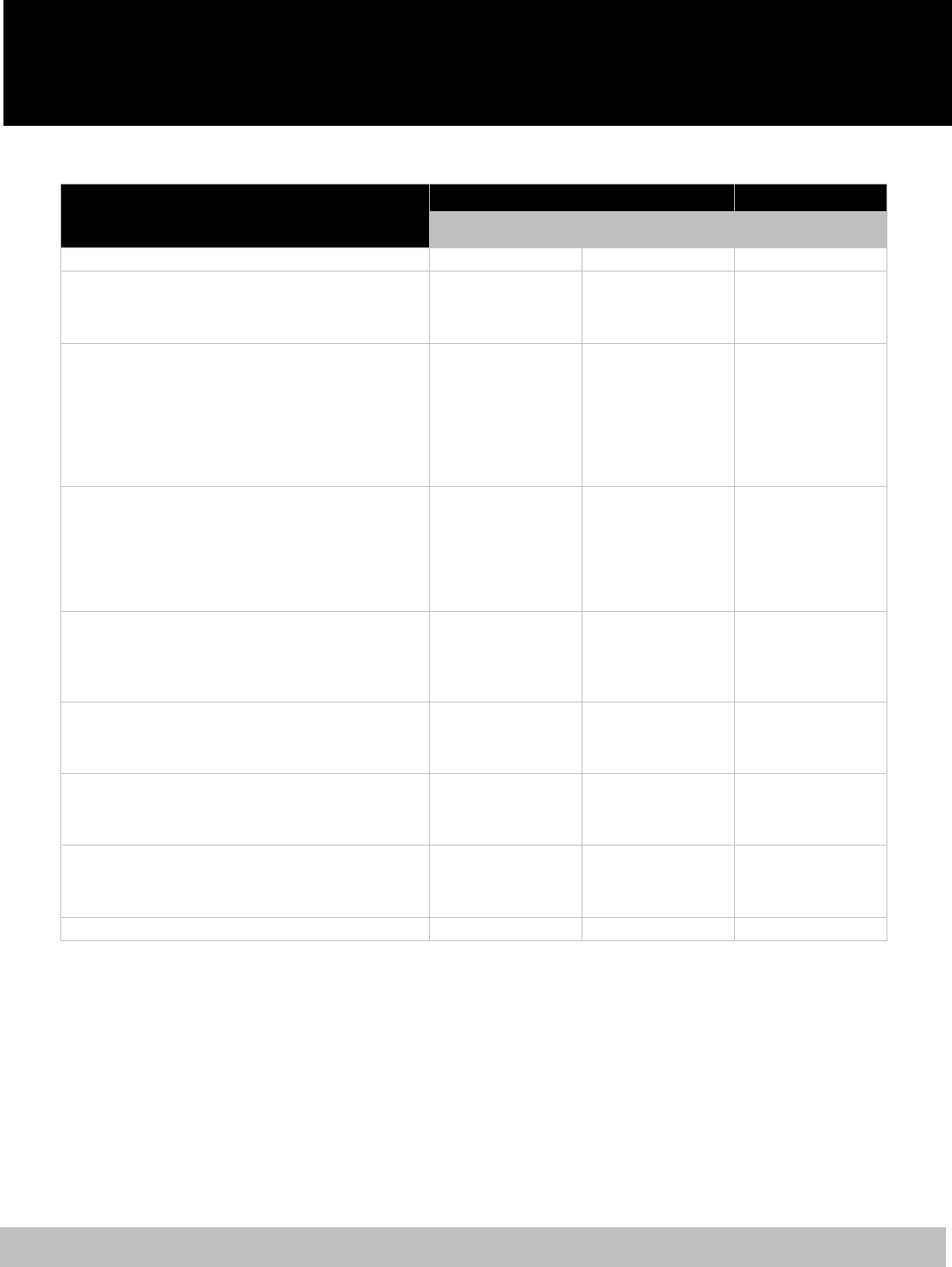
Qualifying Life Event Forms Required Deadline to Add
Newborn/adopted child
Social Security card*
Birth certificate/registration* or
Legal court documentation
60 days from the date of birth or adoption
Legal guardianship/custody
Social Security card*
Legal court documentation
60 days from the court award of legal
guardianship
Spouse
Social Security card
Marriage certificate
60 days from the date of marriage
Loss/gain of coverage
Insurance cancellation form or
COBRA notice
60 days from the date of loss/gain of
coverage
* If you cannot provide a copy of the Social Security card and a birth certificate or birth registration within
the 60-day time frame, you may enroll your newborn with evidence that you have applied for a social
security number and a birth certificate or birth registration. You must provide the social security card and
birth certificate or birth registration to ERSC upon receipt. Failure to provide this information in a timely
manner will result in termination of coverage.
Coverage for your newborn/newly adopted
dependent child(ren) will be retroactive to the
date of birth, adoption, or legal guardianship
when forms are submitted within the 60-day
time frame.
If ERSC receives all required documentation by
the 20
th
of the month, coverage for your new
dependent will begin on the first day of the
following month. If ERSC receives the forms
and necessary documents after the 20
th
of the
month, coverage for your new dependent will
start on the first day of the second month.
If you do not enroll your new dependent within
the 60-day time frame listed above, you must
wait until a future Open Enrollment to enroll
him or her using the BES.
CHANGES IN OR CANCELLATION
OF COVERAGE
In general, you are not permitted to make
changes to your benefits plan during the plan
year. You may make changes to your benefits
plan during the annual Open Enrollment held
each fall.
Certain benefit changes may be made during the
plan year if you experience a qualifying life or
work event. Qualifying life or work events
include:
Marriage/divorce
Birth of child; adoption or legal
guardianship
Death

2024
EMPLOYEE BENEFIT SUMMARY
4
Aging off plan
Change of work status (e.g., you are a .4
paraeducator, not benefits eligible, and your
hours increase to .6—you now are benefits
eligible)
Loss of non-MCPS coverage
Changes due to qualifying life or work events
may be made during the plan year, as described
in the section Enrolling New Dependents.
You may cancel your coverage at any time, but
you may
not cancel your dependent’s coverage
witho
ut proof that the dependent has coverage
elsewhere. It is recommended that you
notify
ERSC promptly because removing a
dependent could change your coverage level
and reduce your
cost. You must provide
evidence o
f other coverage in order to drop a
dependent from coverage.
Also, while you may add or drop yourself, a
spouse, or dependent(s) from your benefits plan
outside of Open Enrollment due to a qualifying
event, you may not make changes to your
benefits plan outside of Open Enrollment. This
means you may not change insurance plans or
cancel individual components of your benefit
plan during the plan year.
If you choose to
cancel coverage outside of
Open Enrollment, you must cancel the entire
employee benefit plan—with the exception of
life insurance coverage(s).
To cancel or change coverage due to a
qualifying life event outside of Open
Enrollment,
you must visit the Employee Self-
Service web page at
www.montgo
meryschoolsmd.org/departments/er
sc/employees/employee-self-service/ and click on
the Benefits enrollment/changes due to a
qualifying life event
link. You have 60 days
from the date of the qualifying event to enroll
and submit the req
uired supporting
documentation to ERSC. You must either
upload this information to the BES when you
enroll or mail it to ERSC.
If ERSC
receives all required documentation by
the 20
th
of the month, changes to or cancellation
of your coverage will become effective on the
first day of the following month. If ERSC
receives the forms after the 20
th
of the month,
changes to your coverage will become effective
on the first day of the second month.
If you do not enroll and provide the necessary
documentation within the 60-day period, you
must wait until a future Open Enrollment to
make any changes using the BES.
Remember: It is your responsibility to
promptly notify ERSC of any changes to your
personal information (e.g., name or address)
or coverage needs.
Loss of Non-MCPS Coverage
You may enroll in an MCPS-provided benefits
plan during the plan year if you or your benefits-
eligible dependents lose coverage provided by a
business or organization other than MCPS. Your
benefits coverage will be effective the first of
the month following your enrollment.
PAYING FOR COVERAGE
You pay for your health plan coverage with
premiums deducted from your paycheck on a
pretax basis. Your premiums are deducted
before income and payroll taxes are calculated,
and your deductions are taken in equal amounts.
The detailed cost is shown on your ePaystub.
Ten-month employees have deductions
taken from 20 paychecks during the school
year.
Twelve-month employees have deductions
taken from 26 paychecks.
Refer to the rate chart at the end of this
document for the base health coverage costs for
2024.
WHEN BENEFITS COVERAGE ENDS
If you terminate employment with MCPS,
benefits coverage for you and any covered
dependents ends on the last day of the month
you terminate employment.

2024
EMPLOYEE BENEFIT SUMMARY
5
Dependent life insurance coverage for a
dependent child automatically ends on
September 30 following the child’s 23
rd
birthday. For dental and vision plans, benefits
coverage for a dependent child automatically
ends at the end of the month in which he/she
turns age 24. For medical and prescription plans,
a dependent child’s coverage automatically ends
at the end of the month in which he/she turns
age 26.
Special Rule for 10-month
Employees
If you are a 10-month employee and you
terminate employment with MCPS at the end of
a school year (on your last duty day based on
your work schedule), your coverage continues
through September 30 because you have prepaid
for benefits through the summer.
CONTINUATION OF BENEFITS
(COBRA)
If your coverage ends, you and your dependents
may be eligible to continue coverage as provided
under COBRA.
You and/or your dependents may become
eligible for coverage under COBRA if you
terminate employment or you and/or your
dependents become ineligible for coverage
under the MCPS benefits plan. You may
continue coverage by paying the full cost of
coverage plus a 2 percent administrative fee for
a period legally-mandated by COBRA
regulations (generally 18–36 months).
MCPS does not share the cost of COBRA
coverage. A COBRA rate chart can be found on
the ERSC website. You will receive a qualifying
event notice (QEN) from the MCPS third party
administrator.
INSURANCE COVERAGE WHILE
ON LEAVE
If you are on an approved leave of absence, you
may elect to continue or terminate your coverage
under the MCPS employee benefit plan.
Depending
on the type and duration of your
leave of absence, you may be required to pay
either the employee share or the full cost of
coverage. For most unpaid leave categories,
there is not an MCPS subsidy, and you are
responsible for 100 percent of the cost of
insurance while on leave. More information
regarding leave of absence policies is available
on the ERSC website at
www.montgomeryschoolsmd.org/departments/er
sc/employees/leave/.
You may elect to terminate coverage by
indicating your choice on the appropriate BES
screen(s). If you wish to continue coverage
while on leave, no action is required.
You can continue life insurance coverage
without continuing medical, dental, vision, or
prescription coverage. If you elect to continue
life insurance coverage, you will be billed by the
MCPS Division of Controller. Failure to pay the
required premium will result in cancellation of
coverage.
Please be advised that if you terminate your
coverage while on leave and, after returning to
work, wish to re-enroll in benefits, you must do
so within 60 days of returning to active work
status. You must re-enroll in the same coverage
you had prior to going on leave. If you had
covered dependents prior to going on leave, the
same dependents will remain eligible for re-
enrollment. If you marry, have a child, or adopt
a child while on leave, they may be added to
your plans with the appropriate qualifying event,
within 60 days of the event. If the birth or
marriage occurred outside of the last 60 days
while on leave, you will need to wait to add the
new dependent during Open Enrollment or when
experiencing another qualifying life event.
In most cases, you cannot continue your
participation in a flexible spending account
(FSA) while on leave. Your FSAs are cancelled
as of the last deduction taken once you are on
leave, and you must reenroll within 60 days of
returning from leave. You can incur expenses up
to the date your leave begins and have until
April 30 following the plan year to submit
claims for reimbursement.

2024
EMPLOYEE BENEFIT SUMMARY
6
While on an approved leave of absence
protected by the Family and Medical Leave Act
(FMLA), you may choose to re-enroll in an
FSA. To do so, complete and submit MCPS
Form 450-3, Flexible Spending Account Election
to have your FSA contributions direct billed to
you.
If you fail to reenroll in the employee benefit
plan within 60 days of returning to active work
status, you must wait until a future Open
Enrollment. In order to reenroll for basic
employee life insurance or optional employee
and optional dependent life insurance, you and
your spouse must provide evidence of
insurability and be approved by MetLife.
If you are absent from work without approved
leave, you still are required to pay health
insurance premiums. If in any given pay period
you do not have sufficient funds to cover the
cost of your insurance premiums, the premiums
will be withheld from your next paycheck. In the
event of a longer unapproved absence from
work, you will be billed the full cost premium
rate. Please keep in mind that you could
jeopardize your eligibility to continue health
insurance coverage if you are absent without
approved leave. For additional information
about leave of absence policies, visit the ERSC
website at
www.montgomeryschoolsmd.org/departments/er
sc/employees/leave/
OUT-OF-AREA COVERAGE
If you are enrolled in the Kaiser Permanente
Health Maintenance Organization (HMO)
medical plan, any eligible dependents that reside
or attend school outside the service area of the
HMO will be covered only for urgent care or
emergency services.
You are covered anywhere in the world for
emergency and urgent care with your Kaiser
Permanente plan. If you regularly travel to
another service area where you will receive
Kaiser Permanente care, you can get a
health/medical record number and a kp.org
account to seamlessly receive care. When
travelling in an area outside of any Kaiser
Permanente service area, you can get care at a
MinuteClinic® and you will be charged your
standard copay or coinsurance. Learn more at
kp.org/travel. Refer to the HMO summary plan
document for details.
Members of the Cigna OAP (POS) plan or
OAPIN (HMO) plan have access to a national
network of doctors and medical facilities. Both
plans provide in-network benefits should you
and/or your dependents seek medical care while
travelling or living outside the service area. If
you are covered by the Cigna OAP plan, you
also have the option to see a nonparticipating
provider, but your out-of-pocket expense will be
higher if you do. If you receive services from a
provider outside of the network, you will have
to—
pay the provider’s actual charge at the time
you receive care,
file a claim for reimbursement, and
satisfy a deductible and coinsurance.
COORDINATION OF BENEFITS
If you or one of your dependents is covered by
more than one insurance plan, there is an order
of benefits determination established by the
National Association of Insurance
Commissioners. The primary plan will be the
first to consider the medical services rendered
for coverage. Any medical care not covered by
the primary plan in full will be considered for
payment by the secondary plan.
Your employee plan is your primary coverage
over any other plan that covers you as a
dependent spouse.
Birthday Rule
If dependent children are enrolled for insurance
coverage with both biological parents (one
MCPS plan, one non-MCPS plan), the primary
insurance plan for the children is determined by
the birthday of the parents.
The plan of the parent with the birthday that
comes first in the calendar year (month and day
only) is primary for the child(ren). This order of
benefits determination for dependent children is
known as the birthday rule.
2024
EMPLOYEE BENEFIT SUMMARY
7
All medical plans offered by MCPS use the
birthday rule for primary insurance plan
determination. The birthday rule does not apply
to stepchildren. Primary care for dependent
stepchildren is determined by the courts.
ENROLLMENT IN MEDICARE
As an active MCPS employee, if you and/or
your covered dependent(s) are eligible for
Medicare due to age, illness, or disability, you
may defer Medicare Part B enrollment without
penalty as long as you are covered by any active
MCPS medical plan. Deferring Medicare
enrollment will save you the cost of additional
monthly Medicare Part B premiums while
maintaining your MCPS medical coverage.
Enrollment in Medicare Part B will not provide
additional medical coverage beyond what
already is included in all MCPS medical plans.
Therefore, employees typically defer Medicare
Part B enrollment until retirement when deferral
no longer is permitted.
If you and/or your qualified dependent(s) defer
Medicare enrollment, you still will be required
to enroll in Medicare Parts A and B when you
retire and no longer are covered by the active
employee health plan. Enrollment in Medicare
must coincide with your retirement date and is
arranged by contacting the Social Security
Administration at least three months prior to
your retirement. At the time of your retirement,
you must submit a copy of the Medicare card(s)
to ERSC with your retirement papers.
Conveying this information to ERSC will
initiate the necessary process to update your
benefit enrollment and notify the insurance
carriers.
All retirees and dependents covered by any
MCPS retiree medical plan are required to enroll
in Medicare Parts A and B when first eligible to
remain covered by the MCPS plan. Once
enrolled, Medicare will be your primary
insurance, and the MCPS medical plan provides
secondary coverage as a supplement to
Medicare.
If you and/or your dependent(s) become
Medicare eligible at any time du
e to end-stage
renal disease (ESRD), you must notify ERSC at
301-517-8100.
Detailed information about post-retirement
health coverage and Medicare is provided during
the Retirement Informational Sessions offered
by ERSC and also is included in the Retiree
Ben
efit Summary, which is available online at
www.montgomeryschoolsmd.org/uploadedFiles/
retiree_benefit_summary_current.pdf.
Please Note
Application for Medicare Part B is completed through your
local Social Security office or online at:
https://www.ssa.gov/benefits/medicare/

2024
EMPLOYEE BENEFIT SUMMARY
8
Enrollment Basics
USING THE BENEFITS ENROLLMENT
SYSTEM (BES)
Employees who wish to enroll in or make
changes to their benefits either when first hired,
during an annual Employee Benefits Open
Enrollment, or when experiencing a qualifying
life event or returning from long-term leave
must make their elections using the BES. To
access and use the system, visit the Employee
Self-Service (ESS) web page at
www.montgomeryschoolsmd.org/departments/er
sc/employees/employee-self-service/.
If you are a new employee, click on the Benefits
enrollment for new employees link. Those
making changes during Open Enrollment click
on the Open Enrollment link. Those
experiencing a qualifying life event click on the
Benefits enrollment/changes due to qualifying
life event link. Then, log in using your Outlook
username and password and follow the onscreen
instructions.
The BES allows you to quickly and easily
review, update, and confirm your benefit
elections; elect a medical or dependent care
flexible spending account (FSA); and designate
your life insurance beneficiaries. Since it is
online, there are no paper forms to fill out or
send in. You simply make your elections and
submit them with a series of clicks.
SUBMITTING SUPPORTING
DOCUMENTATION
Employees adding a dependent to their benefit
plan—whether during Open Enrollment or due to
a qualifying life event—must submit the
necessary supporting documentation to ERSC.
Supporting documentation may be uploaded
during the online enrollment process via the BES
or mailed or delivered in one of the following
ways:
Email: [email protected]
Mail: 45 W. Gude Drive, Suite 1200,
Rockville, Maryland 20850
Pony mail: ERSC at 45 W. Gude Drive
Fax: 301-279-3651 or 301-279-3642
If you choose to submit supporting
documentation via the BES or email, you must
submit an electronically signed Adobe PDF file.
When submitting hard copies of supporting
documentation, please write your name and
employee identification number in the upper
right corner of each page.
2024
EMPLOYEE BENEFIT SUMMARY
9
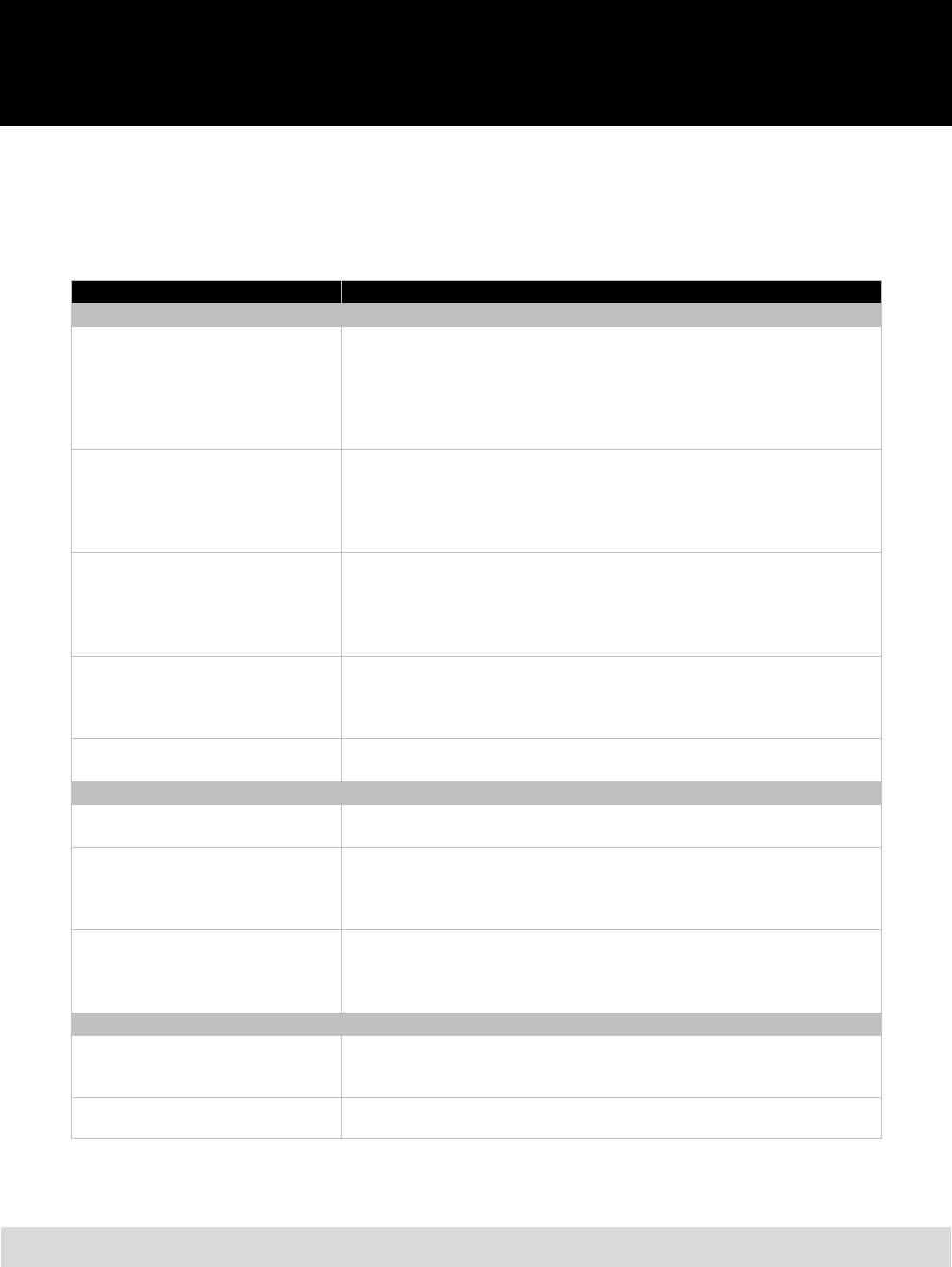
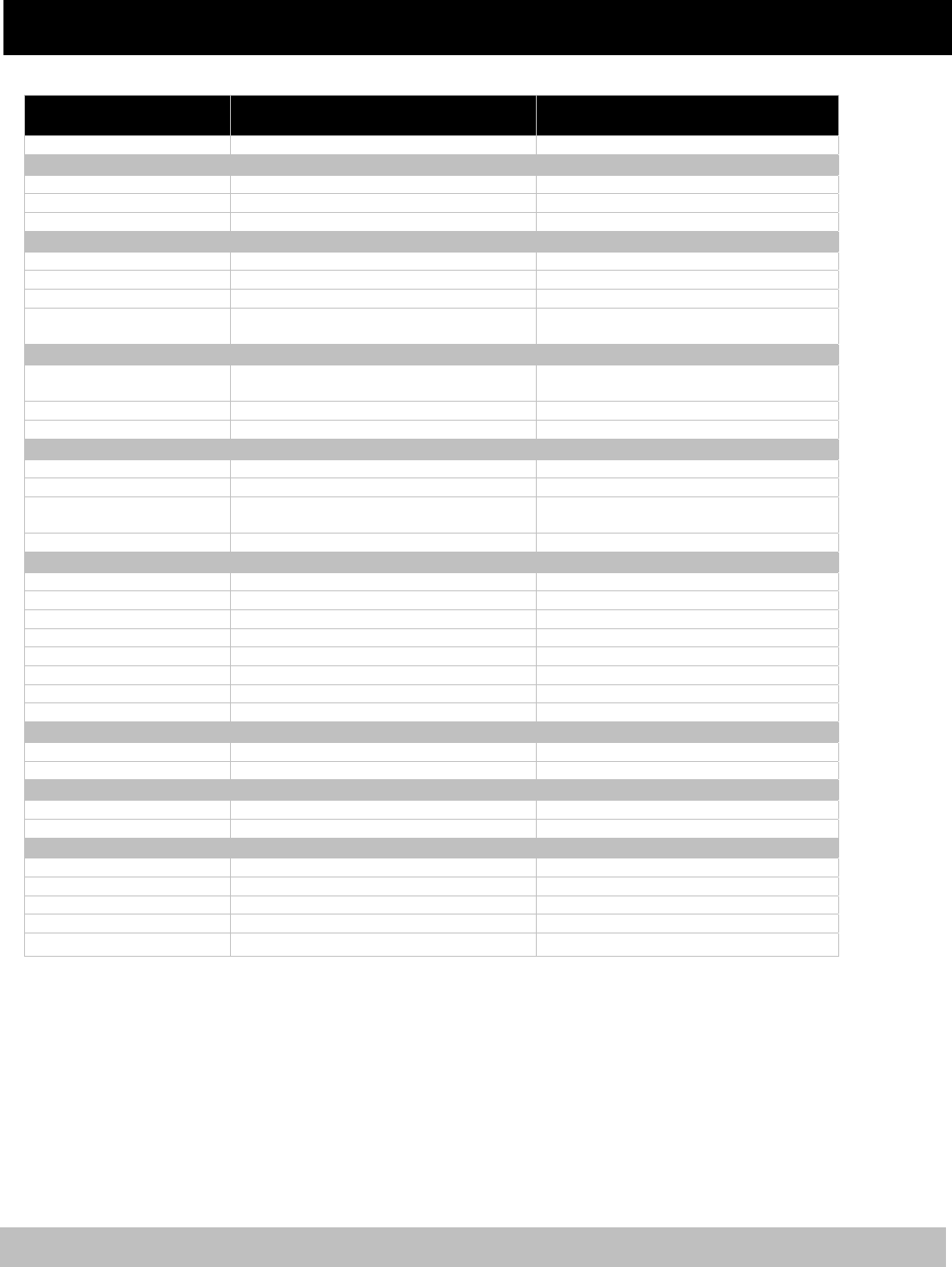
Your Benefits at a Glance
The chart below is a brief overview of your benefit options for 2024. For more information, refer to the
appropriate section in this benefits summary.
Benefit
Y
our Options
Protectin
g
Your Health
Medical
Point-of-Service (POS) Health Plans
Health Maintenance Organizations
(HMO) Health Plans
Cigna Open Access Plus (OAP)
Cigna Open Access Plus In-Network (OAPIN)
Kaiser Permanente HMO
Prescription Drug
CVS Caremark Prescription Drug
(only available to Cigna plan participants)
Kaiser Permanente Prescription Drug
(only available to Kaiser Permanente plan participants)
Dental
CareFirst Preferred Dental Plan (PPO)
Aetna Dental Maintenance Organization (DMO)
Kaiser Permanente Preventive Dental Coverage
(included in medical plan; available only to Kaiser Permanente medical plan
participants)
Vision
Davis Vision (provided through CareFirst)
Kaiser Permanente Vision Plan
(included in medical plan; available only to Kaiser Permanente medical plan
participants)
Wellness Initiatives
Health Risk Assessments
Biometric Health Screenings
Protecting Your Income
Flexible Spending Accounts
Medical spending account (up to $3,050/year)
Dependent care account (up to $5,000/year or $2,500/year if filing separately)
Basic Term Life Insurance
MetLife—
Employee (83 percent paid by MCPS)—2 times annual salary
Dependent (paid by MCPS)—$2,000/spouse, $1,000/each eligible dependent
child up to age 23
Optional Life Insurance
MetLife—
Employee—1 times annual salary (paid by employee)
Dependent—$10,000/spouse or each eligible dependent child (paid by
employee)
Protectin
g
Your Future
Defined Contribution Plans
403(b) Tax Sheltered Savings Plan
457(b) Deferred Compensation Plan
Fidelity—You can elect a percentage of your gross bi-weekly pay or a flat dollar
amount to contribute to one or both plans up to annual IRS limits (available at
www.netbenefits.com/mcps)
Defined Benefit Pension Plans
By completing the appropriate forms, you are enrolled in state and/or county-
sponsored pension plans.

2024
EMPLOYEE BENEFIT SUMMARY
10
Wellness Initiatives
To develop a culture of wellness within MCPS,
the Wellness Initiatives program was established
as part of the school system’s benefit program.
Expanding the efforts of the MCPS employee
wellness program, Well Aware, the program is
intended to educate employees about their health
while offering incentives to those who
participate. Wellness Initiatives is in accordance
with Montgomery County Education
Association (MCEA), Service Employees
International Union (SEIU) Local 500, and
Montgomery County Association of
Administrators and Principals (MCAAP)/
Montgomery County Business and Operations
Administrators (MCBOA) contracts.
Each year, if you are covered by an MCPS-
provided medical insurance plan through Cigna
or Kaiser Permanente, you can reduce your
contributions to your health insurance by
completing a biometric health screening and/or
an online health risk assessment. You must
complete them between the first day of fall
Open Enrollment and the Friday before the
next Open Enrollment begins a year later.
Once you have completed your biometric health
screening and/or health risk assessment, the
incentive(s) will go into effect January 1 of the
calendar year that follows the deadline.
BIOMETRIC HEALTH SCREENINGS
Biometric health screenings monitor for disease
and assess risk for future medical problems. By
completing a biometric health screening of your
blood pressure, blood sugar, body mass index
(BMI), and cholesterol, you will be eligible for a
1 percent increase in MCPS contributions
toward your health insurance. This means that
your contribution to your health insurance will
be reduced by 1 percent if you complete the
biometric screenings within the above time
frame. Your health screening may be completed
by your primary care physician or at one of your
medical plan’s health screenings sponsored by
Well Aware.
Note to Kaiser Permanente plan members:
You must log in
to the Kaiser Permanente website
at www.webmdhealth.com/kp/750/landing to
confirm your participation in the Wellness
Initiatives program and determine if you must
meet any additional requirements.
HEALTH RISK ASSESSMENTS
Health risk assessments are online surveys that
ask basic health
and lifestyle questions to
provide you with a baseline of your current
health status. If you complete a health risk
assessmen
t by the deadline, your contribution to
your health insurance will be reduced by 1
percent.
Your online health risk assessment must be
completed through the medical plan in which
you are enrolled. If you have not already done
so, you will need to create an online account
with
your medical plan. To set up your account,
visit your medical
plan’s website (listed below)
and complete a simple registration process:
• Cig
na—www.MyCigna.com
• Kaiser Permanente—www.kp.org
MCPS will not receive the results of your
biometric health screening or health risk
assessment. Your health insurance carrier will
only indicate whether you have completed your
screening and/or assessment. Your personal
information is protected by the federal Health
Information Portability and Accountability Act.
Medical Coverage
You may choose one of the following medical
plan options:
Point-of-Service (POS) option:
Cigna Open Access Plus (OAP)
Health Maintenance Organization (HMO)
options:
Cigna Open Acce
ss Plus In
-Network
(OAPIN)
Kaiser P
ermanente HMO

2024
EMPLOYEE BENEFIT SUMMARY
11
P
OINT-OF-SERVICE PLAN
A POS plan combines features of an HMO and
an indemnity plan. You receive care in one of
two ways. There is an in-network HMO-like
component offering a full range of services
provided or authorized by your primary care
physician or by an in-network specialist. In
addition, there is an out-of-network component
similar to traditional indemnity insurance. The
out-of-network benefit provides payment for
treatments received from non-network
physicians or specialists after the coinsurance
and a yearly deductible are met. You also will be
responsible for any amount above the usual,
customary, and reasonable (UCR) charges
determined by the plan.
The POS plans do not require you to obtain a
referral to visit a participating in-network
physician or specialist for medically necessary
care.
Cigna Open Access Plus (POS Plan)
MCPS offers this POS plan to employees and
their eligible dependents through Cigna. Cigna
Open Access Plus (OAP) is designed to provide
the highest quality healthcare while maintaining
the freedom to choose from a wide selection of
personal physicians. You have the option to
choose a PCP who specializes in one of these
areas: family practice, internal medicine, general
medicine, or pediatrics. Your PCP or personal
physician can be a source for routine care and
for guidance if you need to see a specialist or
require hospitalization. To access an online
provider directory, please visit www.cigna.com.
With this plan, you have the option to go to any
medical person and facility. However, when
choosing the providers in the OAP network,
your benefit coverage will be greater than opting
to receive services outside the network.
Cigna OAP provides well-managed services to
deliver cost-effective, quality care through the
physicians’ private offices and facilities. To
ensure full and proper medical treatment, and
reduce unnecessary procedures, this plan
emphasizes preadmission screening and prior
authorization for specific services.
As a participant in this plan, you have access to
Cigna’s national network of doctors and
facilities. The availability of a national network
allows access to in-network care for members
wherever you are in the country, when traveling,
and for dependent children when they are living
out of state.
Diabetic supplies are covered under the
prescription drug benefit administered by
CVS/Caremark. Refer to the POS comparison
chart later in this document for more details.
HEALTH MAINTENANCE
ORGANIZATIONS
A health maintenance organization (HMO) plan
offers a full range of services provided by your
PCP or by an in-network specialist. You may
receive benefits only for medical services and
supplies received from a network provider,
except in a true emergency. However, you do
not have to meet a deductible before the plan
pays benefits.
Refer to the HMO comparison chart outlined
later in this document for further details.
Cigna Open Access Plus In-Network
(HMO Plan)
The Cigna Open Access Plus In-Network
(OAPIN) option allows participants to visit any
Cigna network provider without a referral.
Cigna offers access to care from participating
physicians and facilities, with low out-of-pocket
expenses. You may have the option to choose a
PCP to coordinate your care, and pay only a
copayment for most services. You do not have to
complete a claim form.
As a participant in this plan, you have access to
Cigna’s national network of doctors and
facilities. The availability of a national network
allows access to in-network care for members
wherever you are in the country, when traveling,
and for dependent children when they are living
out of state.

2024
EMPLOYEE BENEFIT SUMMARY
12
In addition, Cigna offers member discounts on
fitness, nutrition, and weight management
programs. For more information on discounts,
visit the MCPS Well Aware web page and
navigate to the Discounts tab.
Kaiser Permanente HMO
Kaiser Permanente brings your doctors,
specialists, pharmacy, labs, X-rays, and medical
facilities under one plan. There are more than 33
medical centers within the MCPS service area.
Included are 14 Urgent Care locations, six of
which are Advanced Urgent Care centers open
24/7. You have the choice of more than 1,600
physicians in 50+ specialties from which to
choose. You may receive information about
locations at www.kp.org/locations or by
telephoning 1-800-777-7902. Medical centers
are staffed by doctors, nurses, and specialists
and offer a wide range of services such as
pharmacy, laboratory, X-ray, ambulatory
surgery, and health education. We encourage
you to select a center and PCP that best meets
your needs when you enroll in the plan. If you
do not choose a center, Kaiser Permanente
automatically will assign a center nearest to your
residence of record. You may change your
doctor anytime.
When scheduling an appointment, be sure to ask
for your PCP. You may call and change your
PCP or medical center location at any time.
Each of your covered family members may
select a center and PCP of their choice. Your
PCP is responsible for coordinating all health
needs including hospital and specialty care if
needed. If you enroll in the Kaiser Permanente
HMO, your prescription drug benefits and
diabetic supplies are provided under this plan.
Kaiser Permanente covers diabetic supplies and
provides certain discount specialty services.
Refer to the HMO comparison chart for more
information about the HMO plans.
PREVENTIVE CARE SERVICES
As a result of the Patient Protection and
Affordable Care Act, certain preventive care
procedures no longer will have copays when
they are provided by in-network providers,
regardless of your medical plan choice. The
specific procedures provided for adults and
children are listed separately in the following
charts. Preventive care procedures not listed
specifically will be covered by in-network
providers with copays outlined in the HMO and
POS comparison charts on the following pages.
Out-of-network coverage remains unchanged,
and copays are listed in the POS comparison
chart later in this document.
2024
EMPLOYEE BENEFIT SUMMARY
13
Preventive Services Covered with Zero Copay for Adults*
Preventive Service Covered Who is Eligible, Additional Details
Abdominal Aortic Aneurysm Screening one-time screening for men of specified ages who have ever smoked
Alcohol Misuse Screening and Counseling all adults
Aspirin Use men and women of certain ages
Blood Pressure Screening all adults
Cholesterol Screening adults of certain ages or at higher risk
Colorectal Cancer Screening adults over 50
Depression Screening all adults
Type 2 Diabetes Screening adults with high blood pressure
Diet Counseling adults at higher risk for chronic disease
HIV Screening
all adults at higher risk
Immunizations for:
Hepatitis A
Hepatitis B
Herpes Zoster
Human Papillomavirus
Influenza
Measles, Mumps, Rubella
Meningococcal
Pneumococcal
Tetanus, Diphtheria, Pertussis
Varicella
doses, recommended ages, and recommended populations vary
Obesity Screening and Counseling all adults
Sexually Transmitted Infection (STI) Prevention Counseling adults at higher risk
Tobacco Use Screening all adults and cessation interventions for tobacco users, expanded
counseling for pregnant tobacco users
* Using in-network providers only
2024
EMPLOYEE BENEFIT SUMMARY
14
Preventive Services Covered with Zero Copay for Women *
Preventive Service Covered Who is Eligible, Additional Details
Annual well-woman visit all women
Syphilis Screening all pregnant women, all adults at higher risk
Anemia Screening pregnant women, on a routine basis
Bacteriuria Urinary Tract or Other Infection Screening pregnant women
BRCA Counseling about Genetic Testing women at higher risk
Breast Cancer Mammography Screenings women over 40, every 1 to 2 years
Breast Cancer Chemoprevention Counseling women at higher risk
Breast Feeding Interventions women (to support and promote breast feeding)
Breast Feeding Support, Supplies, and Counseling women (to support and promote breast feeding)
Cervical Cancer Screening sexually active women
Chlamydia Infection Screening younger women and other women at higher risk
Contraceptive Methods and Counseling (FDA-approved**),
including:
Female Condom (OTC)
Diaphragm (P) with Spermicide (OTC)
Sponge (OTC) with Spermicide (OTC)
Cervical Cap (P) with Spermicide (OTC)]
Spermicide (OTC)
Oral Contraceptive (P)
Combined Pill
Progestin
Extended/Continuous
Patch (P)
Vaginal Contraceptive Ring (P)
Shot/Injection (P)
Morning After Pill (over 17 years of age OTC; under
17 years of age P)
IUD (P)
Implantable Rod (inserted by doctor)
Sterilization Surgery
Sterilization Implant
(OTC) Over the Counter
(P) Prescription Required
all women
Folic Acid Supplements women who may become pregnant
Gonorrhea Screening all women at higher risk
Gestational Diabetes Screening pregnant women
Hepatitis B Screening pregnant women at their first prenatal visit
Human Immunodeficiency Virus (HIV) Counseling and
Screening
all women, on an annual basis
Human Papillomavirus (HPV) Testing all women
Interpersonal and Domestic Violence Screening and
Counseling
all women
Osteoporosis Screening women over age 60 depending on risk factors
Rh Incompatibility Screening all pregnant women and follow-up testing for women at higher risk
Sexually Transmitted Infections Counseling all women, on an annual basis
* Using in-network providers only
** Includes surgical, prescription, medical, and OTC services/products. Sterilization is considered a contraceptive method.
Abortion IS NOT considered a contraceptive method.
2024
EMPLOYEE BENEFIT SUMMARY
15
Preventive Services Covered with Zero Copay for Children*
Service Who is Eligible, Additional Details
Alcohol and Drug Use Assessments adolescents
Autism Screening children at 18 and 24 months
Behavioral Assessments children of all ages
Cervical Dysplasia Screening sexually active females
Congenital Hypothyroidism Screening
newborns
Developmental Screening
children under age 3, and surveillance throughout childhood
Dyslipidemia Screening children at higher risk of lipid disorders
Fluoride Chemoprevention Supplements children without fluoride in their water source
Gonorrhea Preventive Medication for the Eyes all newborns
Hearing Screening all newborns
Height, Weight, and Body Mass Index Measurements children of all ages
Hematocrit or Hemoglobin Screening children of all ages
Hemoglobinopathies or Sickle Cell Screening newborns
HIV Screening adolescents at higher risk
Immunization Vaccines for:
Diphtheria, Tetanus, Pertussis
Haemophilus Influenzae Type B
Hepatitis A
Hepatitis B
Human Papillomavirus
Inactivated Poliovirus
Influenza
Measles, Mumps, Rubella
Meningococcal
Pneumococcal
Rotavirus
Varicella
children from birth to age 18; doses, recommended ages, and
recommended populations vary
Iron Supplements children ages 6 to 12 months at risk for anemia
Lead Screening children at risk of exposure
Medical History all children, available throughout development
Obesity Screening and Counseling children of all ages
Oral Health Risk Assessment young children
Phenylketonuria (PKU) Screening for Genetic Disorder newborns
Sexually Transmitted Infection (STI) Prevention Counseling adolescents at higher risk
Tuberculin Testing children at higher risk of tuberculosis
Vision Screening children of all ages
* Using in-network providers only
2024
EMPLOYEE BENEFIT SUMMARY
16
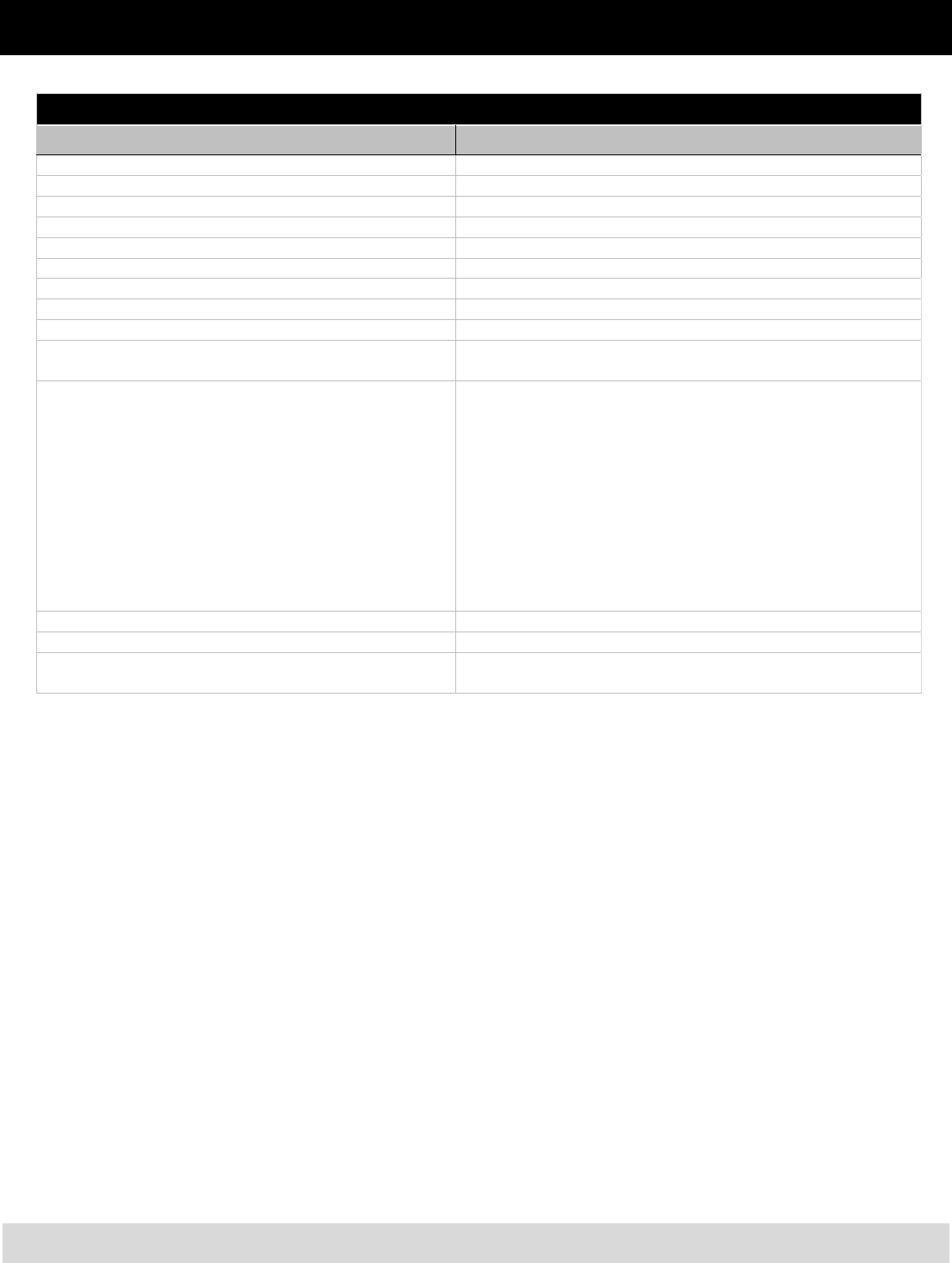
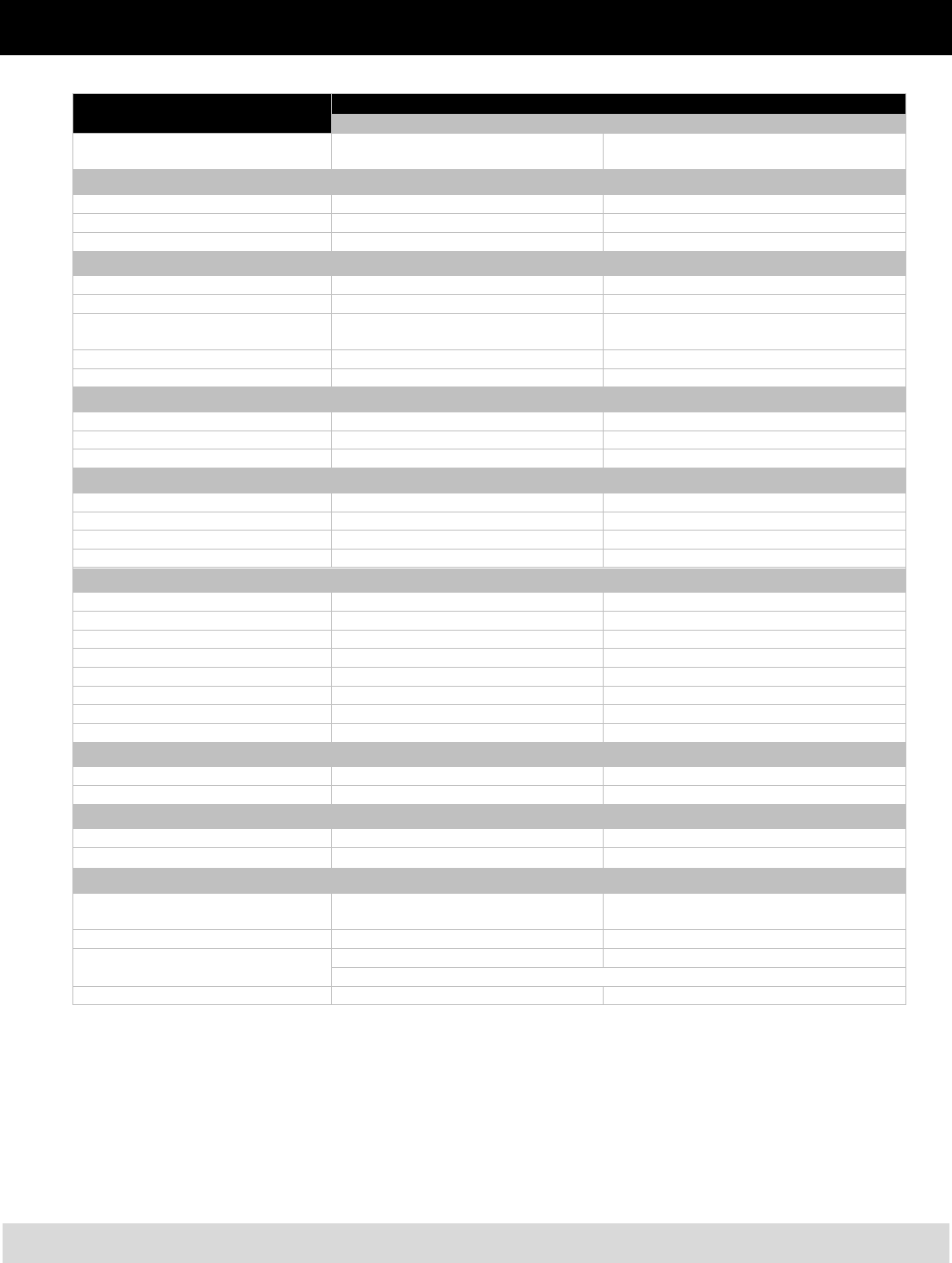
Health Maintenance
Organization (HMO) Plans
Kaiser Permanente HMO Plan
Cigna Open Access Plus
In-Network (OAPIN) Plan
Annual Deductible None None
Preventive Care
Routine Physical Exam Covered in full Covered in full
Well Baby/Child Care Covered in full (under age 5) Covered in full
Childhood Immunizations Covered in full (under age 5) Covered in full
Physician Services
Physician Office Visit $10 copay $10 copay
Specialist Office Visit $20 copay $20 copay
Lab Work and X-rays Covered in full Covered in full
Allergy Shots $10 copay
$10 copay
$20 specialist copay
Maternity Care
Prenatal and Postnatal Care
$10 copay, no charge once pregnancy is
confirmed*
Covered in full
Physician Services Covered in full $10 copay
Hospital Services Covered in full Covered in full
Emergency Services (when medically necessary)
Urgent Care Centers $20 copay $20 copay
Emergency Room $150 copay (waived if admitted) $150 copay (waived if admitted)
Emergency Physician
Services
Covered in full Covered in full
Emergency Ambulance Covered in full if authorized Covered in full
Hospital Services—Inpatient
Semi-Private Room Covered in full Covered in full
Professional Services Covered in full Covered in full
Surgical Procedures Covered in full Covered in full
Specialty Care/ Consultation Covered in full Covered in full
Anesthesia Covered in full Covered in full
Radiology and Drugs Covered in full Covered in full
Intensive Care Covered in full Covered in full
Coronary Care Covered in full Covered in full
Hospital Services—Outpatient
Surgical Procedures $20 copay $20 copay
Professional Fees Covered in full $10 copay/$20 copay for specialist
Mental Health/Substance Abuse Services
Inpatient Days Covered in full Covered in full
Outpatient Visits $10 copay $10 copay
Other Services
Catastrophic Illness Covered in full Covered in full
Durable Medical Equipment Covered in full You pay 25%
Home Health Care Covered in full Covered in full
Hospice Care Covered in full Covered in full
Skilled Nursing Care Covered in full up to 100 days per contract year Covered in full
*Applies to services not specifically listed in the previous preventive care charts.
2024
EMPLOYEE BENEFIT SUMMARY
17
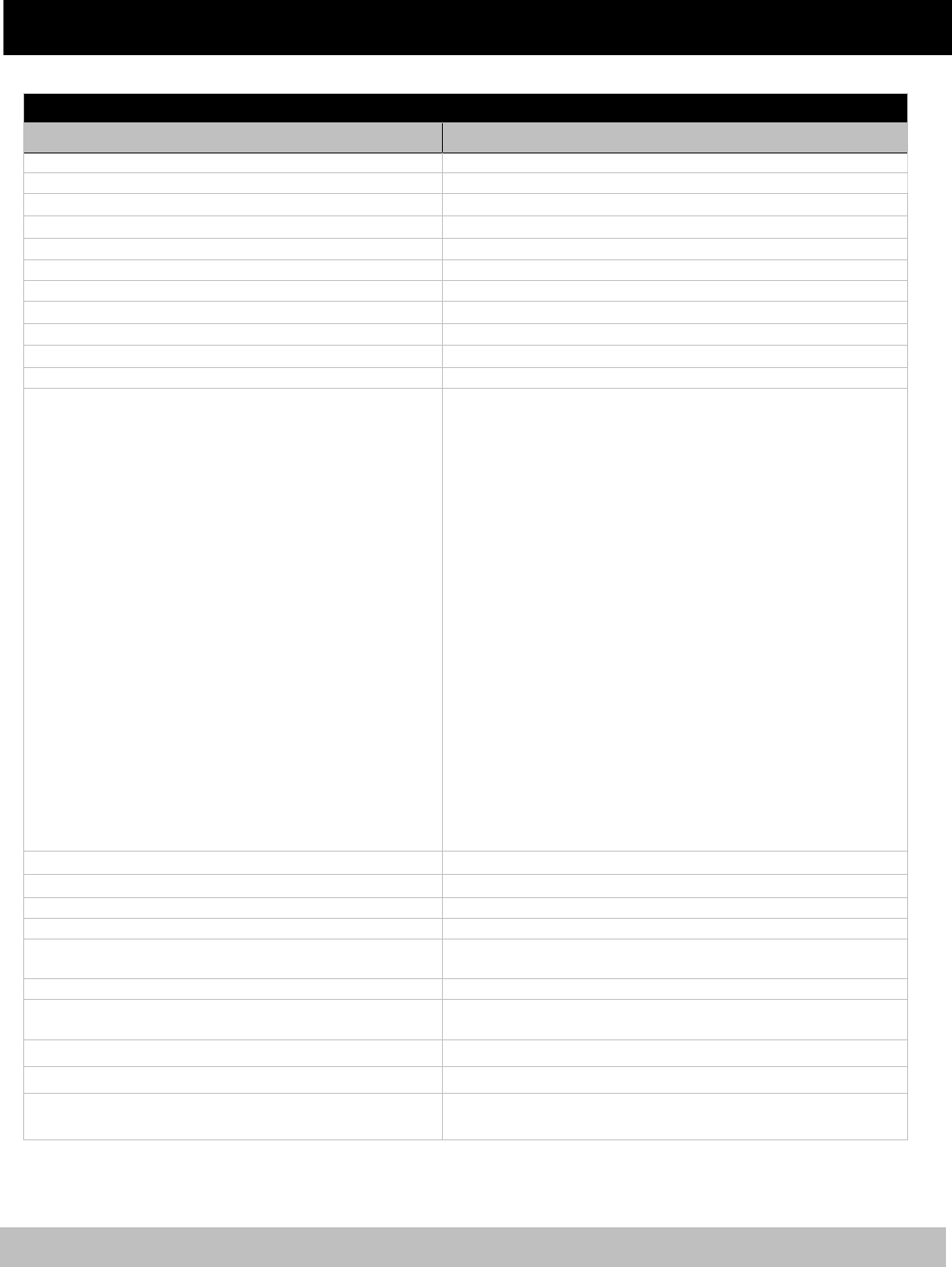
Open Point-of-Service (POS) Plan
Cigna Open Access Plus (OAP) Plan
In-Network Out-o
f
-Network
Annual Deductible None
$300 individual,
$600 family
Preventive Care
Routine Physical Exam $15 copay* Not covered
Well Baby/Child Care $15 copay* 80%, no deductible
Childhood Immunizations Covered in full 80%, no deductible
Physician Services
Physician Office Visit $15 copay 80% after deductible
Specialist Office Visit $25 copay 80% after deductible
Lab Work and X-rays Covered in full
Diagnostic: 80% after deductible
Routine: not covered
Allergy Evaluations $15 copay each visit 80% after deductible
Allergy Shots Covered in full 80% after deductible
Maternity Care
Prenatal and Postnatal Care $25 copay first visit, covered in full after* 80% after deductible
Physician Services Covered in full 80% after deductible
Hospital Services Covered in full 80% after deductible
Emergency Services (when medically necessary)
Urgent Care Centers $25 copay $25 copay, then plan pays 80%
Emergency Room $150 copay (waived if admitted) $150 copay (waived if admitted)
Emergency Physician Services Covered in full Covered in full
Emergency Ambulance Covered in full Covered in full
Hospital Services—Inpatient
Semi-Private Room Covered in full 80% after deductible
Professional Services Covered in full 80% after deductible
Surgical Procedures Covered in full 80% after deductible
Specialty Care/ Consultation Covered in full 80% after deductible
Anesthesia Covered in full 80% after deductible
Radiology and Drugs Covered in full 80% after deductible
Intensive Care Covered in full 80% after deductible
Coronary Care Covered in full 80% after deductible
Hospital Services – Outpatient
Surgical Procedures Covered in full 80% after deductible
Professional Fees Covered in full 80% after deductible
Mental Health/Substance Abuse Services
Inpatient Days Covered in full 80% after deductible
Outpatient Visits $15 copay 80% after deductible
Other Services
Catastrophic Illness Covered in full
Covered in full after $1,000 out-of-pocket expenses
(excludes deductible)
Durable Medical Equipment** Covered in full 80% after deductible
Home Health Care/
Skilled Nursing Care
Covered in full 80% after deductible
(Up to 60 visits for both in- and out-of-network)
Hospice Care Covered in full 80% after deductible
*Applies to services not listed in the previous preventive care charts.
**Does not include diabetic supplies such as lancets, glucose strips, etc.
2024
EMPLOYEE BENEFIT SUMMARY
18
Other Benefit Plan
Coverage
In addition to medical coverage, you may
choose dental, vision, and prescription drug
coverage when you enroll (see the appropriate
section in this document for details). Base rates
for the 2024 plan year, which do not include
Wellness Initiatives credit(s), are included in this
document. Rates that factor in Wellness Initiatives
credits are available during the plan year at
https://www2.montgomeryschoolsmd.org/depart
ments/ersc/employees/benefits/
You are responsible for updating beneficiary
designations for your life insurance plans, the
state and county pension plans, and the defined
contribution plans [403(b) and 457(b)]. You may
update life insurance beneficiary(ies) during
Open Enrollment or if you experience a
qualifying life event during the plan year, by
visiting the Employee Self-Service web page at
https://www2.montgomeryschoolsmd.org/depart
ments/ersc/employees/employee-self-service/ and
selecting the appropriate link under the blue My
Benefits banner. Pension plan forms are
available on the ERSC website. To change your
defined contribution plan beneficiaries, contact
Fidelity directly at 800-343-0860 or
www.netbenefits.com/MCPS.
Dental Coverage
If you are eligible for benefits, you may choose
from the following dental plans:
CareFirst Dental Plan (PPO),
Aetna Dental Maintenance Organization
(DMO), or
Kaiser Permanente medical plan members are
automatically enro
lled in the Kaiser Permanente
dental plan. They have the option of also
enrolling in either the PPO plan or DMO plan.
You may change dental plans only during Open
Enrollment or if a DMO participant and you
move outside of the Aetna DMO service area.
CareFirst Preferred Dental Plan
(PPO)
If you enroll in the CareFirst Dental PPO plan,
you have the freedom to select the dentist of
yo
ur choice. This plan offers in- and out-of-
network benefits.
You can access in-network provider information
by calling 1-888-755-2657 or visiting
CareFirst’s website at
www.carefirst.com/mcps.
Under Find a Doctor, click Search Now.
Log in to My Account.
Select Dental.
Search by Name or Specialty.
You receive a higher level of benefits if you
receive dental services from a participating (in-
network) PPO dentist. If you receive dental
services from a non-participating (out-of-
network) dentist, you receive a less generous
level of benefits. Reimbursement is based on the
schedule of dental benefits and is subject to
deductibles, copays, and reasonable and
customary charges. Prophylaxis, including
scaling and polishing, is covered up to two times
per calendar year.
Orthodontic benefits are available to dependent
children of active employees only if they were
Important Notice
New employees eligible for benefits are enrolled in the
basic term life insurance plan automatically. You will need
to designate a beneficiary for basic life insurance when you
enroll in benefits via the BES. If you wish to decline basic
term life insurance coverage, you must do so online by
electing “decline” life insurance coverage. See the Life
Insurance section of this document for additional details.
You may update your life insurance beneficiaries at any
time by using the BES. Make sure to update beneficiary
designations as your circumstances change.
2024
EMPLOYEE BENEFIT SUMMARY
19
enrolled in the MCPS plan and younger than age
20 when the treatment began. The in-network
orthodontic benefit is 50 percent of the allowed
charge, and the out- of-network orthodontic
benefit is 30 percent of the allowed charge.
There is a maximum lifetime orthodontic benefit
of $1,000 per child (in- or out-of-network).
Aetna Dental Maintenance
Organization (DMO)
If you wish to enroll in the Aetna DMO plan,
you should contact Aetna directly to verify that
you reside in the DMO service area. As a DMO
participant, you must select a primary dentist
from a list of participating DMO dentists and be
on the dentist’s roster before your first
appointment. To obtain information and select
a participating DMO provider, visit Aetna’s
website at www.aetna.com/docfind or call
1-800-843-3661.
The Aetna DMO does not require you to meet an
annual deductible before benefits are paid, and
there is no maximum annual benefit limitation.
However, benefits are paid only if you receive
care from a dentist who is part of the DMO
network. Benefits are paid at a certain
percentage (100 percent for preventive or basic
or 75 percent for major).
Orthodontic benefits are available to dependent
children of active employees only if they were
enrolled in the MCPS plan and younger than age
20 when the treatment began. The orthodontic
benefit is 50 percent of the scheduled fee,
limited to one full treatment per eligible child.
There is no lifetime maximum.
Refer to the chart on the next page for more
information about your dental options.
Kaiser Permanente Dental Plan
The Kaiser Permanente medical and prescription
plan includes a schedule of benefits for in-
network dental care for both adult and pediatric
patients. Participants pay $30 for a dental exam
and cleaning. More extensive care is offered at
fixed fees lower than the usual and customary
charges for dental services. For more information
visit DominionNational.com/KaiserDentists.
This coverage is not available to those who are
not Kaiser Permanente members.
Refer to the chart on the next page for more
information about your PPO and DMO dental
options. For details about the Kaiser Permanente
dental plan, visit
www.montgomeryschoolsmd.org/departments/er
sc/employees/benefits/health/medical/kaiser.aspx
and click on the Evidence of Coverage link.
2024
EMPLOYEE BENEFIT SUMMARY
20
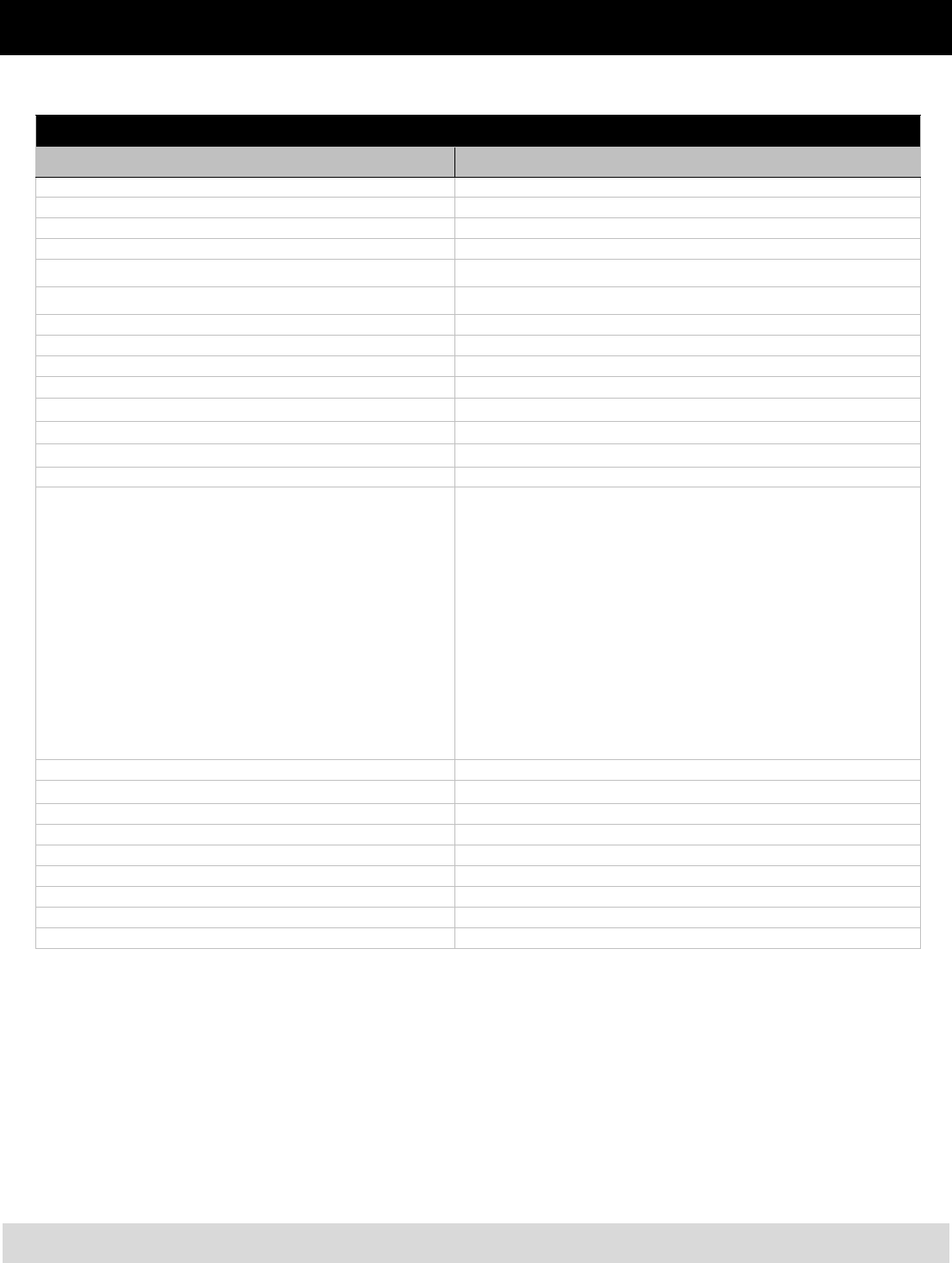
Dental Benefits
CareFirst PPO Aetna DMO
In-Network
Plan pays:
Out-of-Network
Plan pays:
In-Network Only
Plan pays:
Maximum Annual Benefit* $2,000 $2,000 None
Annual Deductible
Class I
Class II
Class III
None
$50
$50
None
$100
$100
None
None
None
Diagnostic (Class I)
Routine exams
X-rays
Prophylaxis (includes scaling and polishing)
Fluoride (one treatment per year up to age 18)
Sealants (one treatment every three years on permanent
molars only under age 16)
Oral Hygiene Instruction
100%
Oral Hygiene
Instruction not covered
80%
Oral Hygiene
Instruction not covered
100%
Basic (Class II)
Amalgam
Composite Filling (anterior tooth only)
Pulp Capping
Root Canal Therapy with X-rays and Cultures (other than
molar root canal)
Scaling and Root Planing
100% 80% 100%
Basic (Class II)
Space Maintainers
Molar Root Canal Therapy
Osseous Surgery (periodontal surgery)
General Anesthesia
100% 80% 75%
Major (Class III)
Inlays, Onlays, and Crowns
Full and Partial Dentures
Bridge Pontics, and Abutments
50%
40%
Maximum eligible charge
per service: $400
75%
Major (Class III)
Surgical Removal of Impacted Teeth
100%
80%
Maximum eligible charge
per service: $400
75%
Orthodontics** (Class IV)
Orthodontic Appliances and Treatment (one lifetime treatment
per covered dependent child only if treatment begins prior to
age 20 while covered under the MCPS plan)
50%, up to $1,000
lifetime maximum
30%, up to $1,000
lifetime maximum
50%, no lifetime
maximum
Dental Implants 50% N/A N/A
*The $2,000 maximum annual benefit is a combined total benefit from in-network and/or out-of-network benefit
total.
** The $1,000 maximum lifetime benefit is a combined total benefit from in-network and/or out-of-network benefit
total.
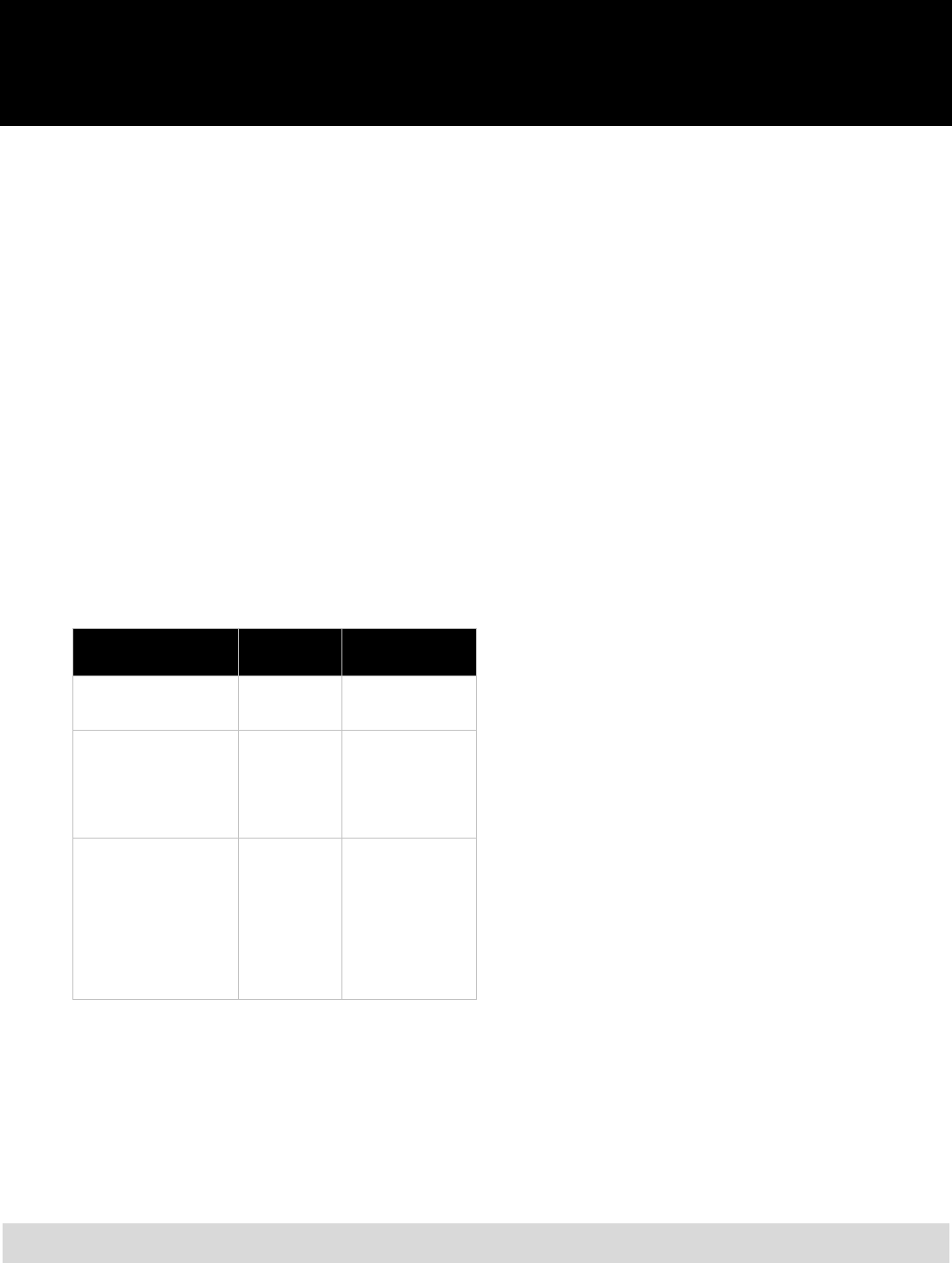
2024
EMPLOYEE BENEFIT SUMMARY
21
Vision Coverage
If you are eligible for benefits, you may choose
to enroll in vision coverage offered by Davis
Vision (provided through CareFirst). Kaiser
Permanente medical plan members are
automatically enrolled in the Kaiser Permanente
vision plan, but have the option of also enrolling
in the Davis Vision plan.
Davis Vision Plan
As a participant in the Davis Vision plan, you
have access to care through either our network of
independent, private practice doctors
(optometrists and ophthalmologists) or select
retail partners for vision services. When you use
a Davis Vision provider, the benefit below is
deducted from eligible expenses at the time the
services are rendered. There is no need to file a
claim.
Service
Maximum
Benefit
Limits
Exams:
Optometrist
Ophthalmologist
$50
$66
One exam during
any consecutive 18-
month period
Frames:
Frames only $40
One set of frames
during any
consecutive 18-
month period
(in lieu of contact
lenses)
Lenses only, per pair:
Single vision
Bifocal
Trifocal
Lenticular
Contact Lenses:
Medically Necessary**
Standard or Disposable
$40
$70
$90
$240
$230
$80
Two lenses during
any consecutive 18-
month period
(in lieu of contact
lenses)
In lieu of lenses &
frames
**Contact lenses are covered up to $230 only if they are
prescribed after cataract surgery or when needed to restore the
visual acuity of the person’s healthier eye to 20/70 or better, and if
this cannot be accomplished with regular glasses. Otherwise, they
are covered at $80 in lieu of glasses.
This coverage does not provide benefits for the
following:
More than one eye examination, including
refraction, and two lenses per person during
any consecutive 18-month period.
More than one set of frames per person
during any consecutive 18-month period.
Services and materials in connection with
special procedures, such as orthoptics and
vision training, or in connection with
medical or surgical treatment of the eye.
Sunglasses, plain or prescription.
Replacement of lost, stolen, or broken lenses
or frames furnished under this benefit.
Eye examinations required by an employer
as a condition of employment, where the
employer is required to provide by virtue of
a labor agreement or a government body.
Any eye care to the extent that benefits are
payable for the service or supply under any
other coverage of the plan, such as
infections of the eye and eye surgery that are
covered under your medical plan.
Value Added Features—Replacement contacts
(after initial benefit) through
www.DavisVisionContacts.com mail order
contact lens replacement service ensures easy
and convenient online
purchasing and quick
shipping direct to your door.
The vision plan enables participants to purchase
lens option
services at discount prices. The plan
also provides LASIK surgery discounts of u
p to
25 percent off the provider’s usual and
customary fees, or 5 percent off advertised
sp
ecials, whichever is lower. For additional
information on LASIK surgery, please call 800-
78
3-5602 for a list of participating Davis Vision
providers.
Out-of-Network Vision Services—Please be
aware that non-Davis Vision providers will
expect the en
tire payment up-front. You may
then seek reimbursement
by submitting a claim
form to Davis Vision. Refer to the benefits chart
at left for reimbursement amounts.
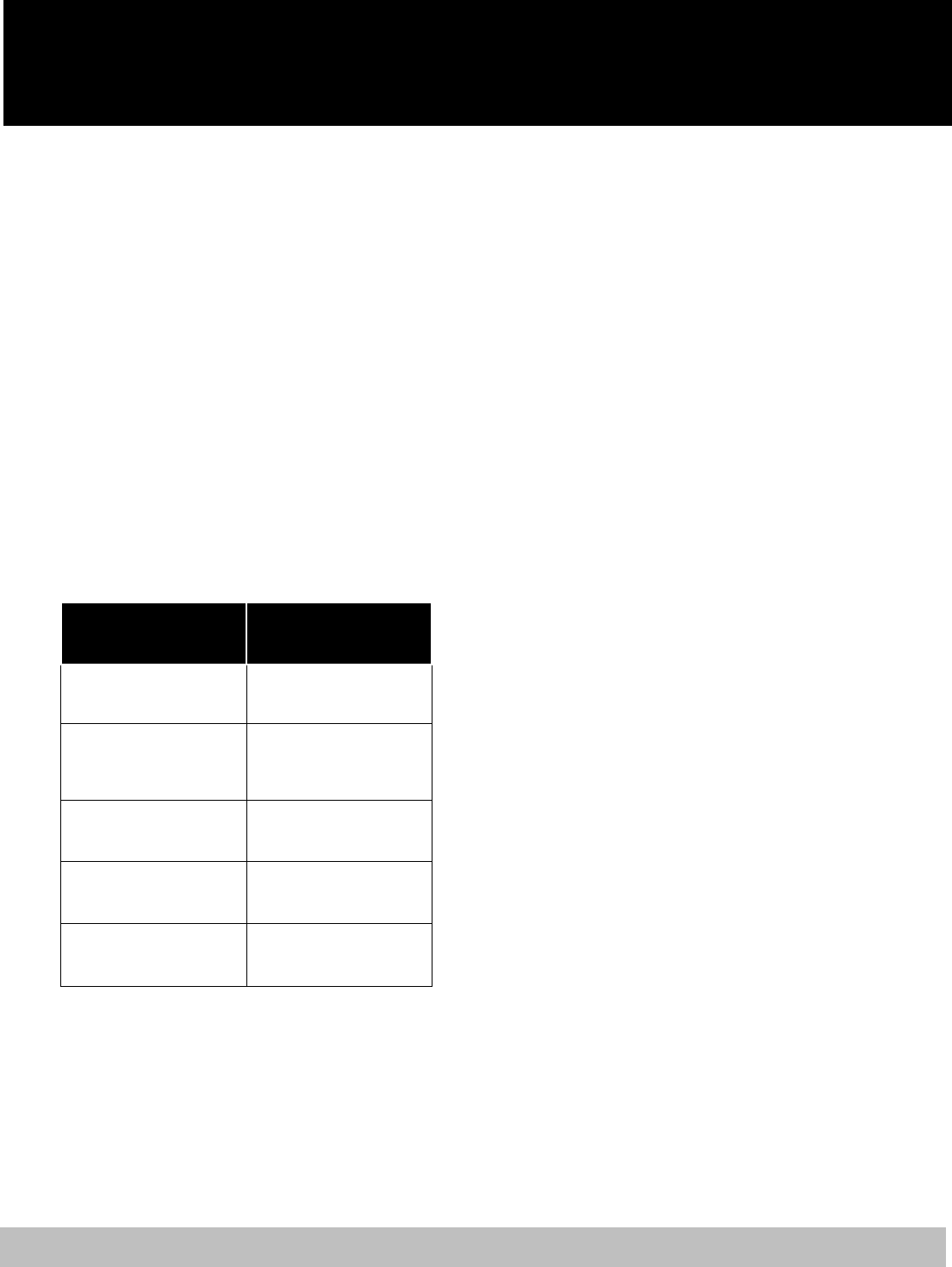
2024
EMPLOYEE BENEFIT SUMMARY
22
Need More Information?—Visit
www.carefirst.com/mcps to access the Davis
Vision website or call 1-800-783-5602. Hours of
operation are—
Monday–Friday, 8:00 a.m.–8:00 p.m.
Saturday, 9:00 a.m.–4:00 p.m.
Kaiser Vision Plan
In addition to medical and prescription coverage,
Kaiser Permanente offers a vision program included
in the plan premium. For details about this vision
plan, visit
www.montgomeryschoolsmd.org/departments/er
sc/employees/benefits/health/medical/kaiser.aspx
and click on the Evidence of Coverage link. You
will find the vision plan information on page
118. The in-network-only benefits are as follows:
The in-network-only benefits are as follows:
KAISER PERMANENTE
VISION PLAN
COPAYS
Exams:
Optometrist
Ophthalmologist
$10 per visit
$15 per visit
Lenses and frames:
(Limited to a select group)
$75 discount off retail price
combined for lenses and
frames purchased at
KP Optical
Contact lenses:
(Limited to a select group)
$25 discount off retail price
for contact lenses purchased
at KP Optical
Medically necessary
contact lenses:
(Limited to a select group)
No charge, limited to two pair
per eye, per year
Low vision aids:
(Unlimited low vision aids
from available supply)
No charge
Vision benefits are provided by Vision
Essentials. There are 18 Vision Essential
locations in the MCPS service area. For more
information and a list of the Vision Essentials
locations near you, visit kp2020.org.
Prescription Drug
Coverage
Two prescription drug plans are offered to
MCPS employees. Eligibility for a plan depends
on which medical plan you choose. If you enroll
in a Cigna medical plan, or if you decline
medical coverage, you are eligible to enroll in
the CVS/Caremark prescription drug plan.
If you enroll in the Kaiser Permanente HMO,
you must enroll in the Kaiser Permanente
prescription drug plan to receive a prescription
drug benefit.
CVS/Caremark Prescription Plan
The CVS/Caremark prescription plan provides
benefits for short-term medications to be filled at
participating retail pharmacies using the
CVS/Caremark prescription drug card. Short-
term medications are medicines prescribed for
short-term illnesses such as a cold, flu, or
infection, generally requiring no more than a 30-
day supply.
Filling prescriptions for long-term maintenance
medications works differently. Long-term
maintenance medications generally are used to
treat long-term chronic conditions such as high
blood pressure, arthritis, coronary artery disease,
and diabetes.
To avoid paying penalty fees, you must fill your
long-term maintenance medications in 90-day
increments. You are allowed one initial fill and
one refill at any participating retail pharmacy.
After that, you only may fill your 90-day supply
of long-term maintenance medications at a CVS
pharmacy or through the CVS/Caremark Mail
Service pharmacy. Some long-term medications
will be subject to the specialty drug guideline
management program or the generic drug step
therapy program. Refer to the sections “Specialty
Drug Coverage” and “Generic Drug Step
Therapy” for information about each program.
The plan has a three-tier copay structure and
provides financial incentives for using generic
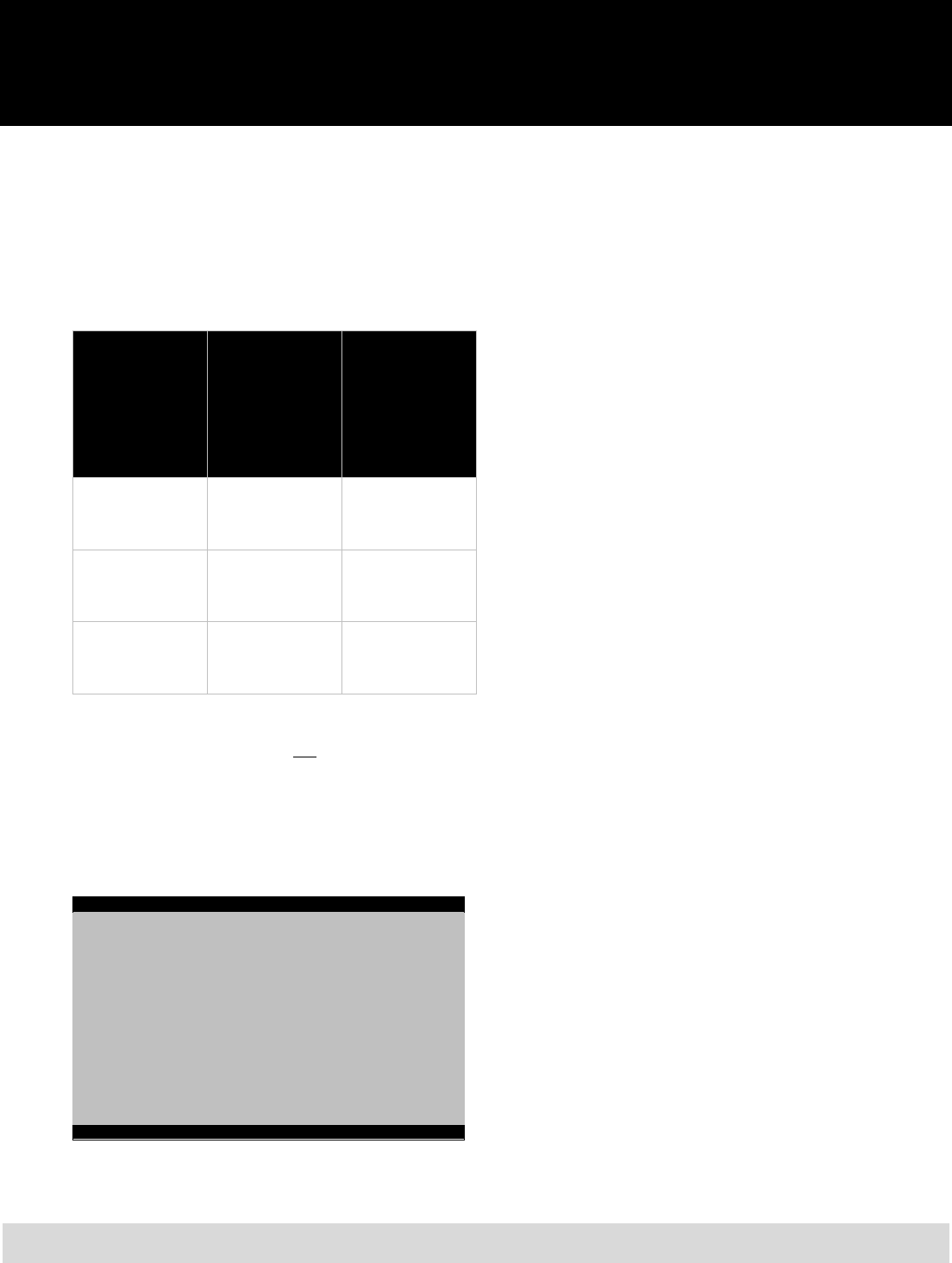
2024
EMPLOYEE BENEFIT SUMMARY
23
drugs, using preferred brand name drugs, and
purchasing maintenance medications through
CVS/Caremark’s Mail Service and CVS retail
pharmacies. These copay structures will only
apply to those drugs not subject to the specialty
drug guidelines or generic drug step therapy.
Refer to the chart below for more information:
Retail
(up to 30-day
supply)
CVS/Caremark
Mail Service
Pharmacy or
CVS retail
pharmacy
(up to 90-day
supply)
Generic $10 copay
One refill allowed
for maintenance
medications
$10 copay
Preferred Brand
Name (no generic
equivalent)*
$25 copay
One refill allowed
for maintenance
medications
$25 copay
Non-Preferred
Brand Name**
$40 copay
One refill allowed
for maintenance
medications
$40 copay***
*Detailed information is available on the CVS/Caremark website.
**If you purchase a brand name drug when a generic equivalent
exists, you pay the generic drug copay plus the difference
between the non-preferred brand name drug and generic drug
cost. Example: Generic drug cost is $100, Non-Preferred Brand
Name drug cost is $200, and your copay is $110.
***There is no penalty for purchasing a brand name drug that has
a generic equivalent if a letter of medical necessity is filed. See
details on following page.
Please Note
You can purchase your 90-day supply of maintenance
medication at a CVS pharmacy for the same copay as the
CVS/Caremark Mail Service pharmacy.
If you choose not to purchase a maintenance medication at
a CVS pharmacy or through CVS/Caremark Mail Service
after two fills at another retail pharmacy, you will pay the
corresponding copay, plus the difference between the mail
order and retail prescription cost.
To take advantage of the lowest copay, choose
generic drugs when available. Plan participants
who choose to purchase a brand name drug
when a generic equivalent exists will be required
to pay the generic drug copay plus the difference
between the cost of the brand name drug and its
generic equivalent.
When your doctor certifies in a letter (along with
your prescription) that it is medically necessary
to prescribe a brand name drug and not its
generic equivalent, if it meets the FDA-approved
diagnosis criteria, you will be charged the brand
name copay, without penalty, for mail order
only.
The letter of medical necessity must be written
on the doctor’s official letterhead (not written on
the prescription) and must contain details of the
medical reason accompanied by the prescription.
Simply stating that in his/her medical opinion
brand name drugs are better than generic drugs
is not sufficient medical documentation.
CVS/Caremark will require yearly updates of
medical necessity.
The letter of medical necessity and prescription
should be sent to:
CVS/Caremark, Inc.
Department of Appeals, MC109
P.O. Box 52084
Phoenix, AZ 85072-2084
CVS/Caremark also can be reached by fax at
1-866-689-3092.
The plan provides two options for the purchase
of brand name drugs that do not have a generic
equivalent:
$25 copay for any preferred brand name
drug that appears on CVS/Caremark’s
Primary Drug list (updated quarterly) or
$40 copay for non-preferred brand name
drugs that do not appear on
CVS/Caremark’s Primary Drug list
Coverage for over-the-counter drugs, cosmetic
drugs, experimental drugs, and vitamins is
excluded under the MCPS plan. While not all
drugs are covered, those that are not may be
filled at 100 percent of the discounted cost.

2024
EMPLOYEE BENEFIT SUMMARY
24
The following medications have prior
authorization requirements, corresponding
programs, or quantity limits:
Anabolic steroids, some treatments for acne,
Botox, growth hormones, and medication to
treat fungal infections all require prior
authorization.
Smoking cessation drugs and weight loss
medications require corresponding
programs.
Drugs for erectile dysfunction have a
quantity limit of six doses per month.
Your doctor will need to contact the prior
authorization staff with your diagnosis. If
you
meet the criteria, your prescription will be
approved. The prior authorization phone number
is 1-800-626-3046. The prior authorization will
be valid through the life of the prescription
(maximum of one year).
Specialty Drug Coverage—Drugs used to treat
certain conditions are considered specialty
drugs. These conditions may include multiple
sclerosis, oncology, allergic asthma, human
growth hormone, Hepatitis C, psoriasis,
rheumatoid arthritis and respiratory syncytial
virus, but other conditions may be included as
well. In an effort to maximize your access to
these drugs as well as the cost-effectiveness to
both you and MCPS, these drugs are subject to
the Specialty Guideline Management Program.
Under this program, you still have access to the
specialty drugs prescribed by your physician.
However, you must go through the proper
process in order to obtain these medications. To
initiate this process, your physician will have to
coordinate with CVS/Caremark in order for
these prescriptions to be filled.
For additional information or to see if your
medication is in this category, call the toll-free
number on the back of your CVS/Caremark ID
card or visit www.caremark.com.
Generic Drug Step Therapy—CVS/Caremark
administers a generic drug step therapy program
as part of its prescription plan to assist you and
MCPS in managing prescription costs. Brand-
name drugs that are used
to treat certain
conditions, including, but not limited to, high
blood pressure and high cholesterol, are subject
to the generic first step therapy requirements.
Be sure to ask your physician whether or not the
drug being prescribed is affected by the generic
drug step therapy program. CVS/Caremark
maintains a list of all affected drug classes on
their website at www.caremark.com.
Primary Preferred Drug List
—For drugs that
are not subject to the specialty guideline
management program or the generic drug step
therapy program, CVS/Caremark offers a
Primary Preferred Drug List. The Primary
Preferred Drug list is a list of preferred brand-
name medications that have been carefully
reviewed and selected by the CVS/Caremark
National Pharmacy and Therapeutics Committee
of practicing doctors and clinical pharmacists for
their safety, quality, and effectiveness. You can
help control the amount you pay for
prescriptions by asking your doctor to prescribe
medications on the Primary Preferred Drug list.
The medicines on the Primary Preferred Drug
list are not equivalents of non-preferred brand-
name medicines, but are medicines in the same
therapeutic category used to treat the same
condition.
Remember, not every drug listed on the Primary
Preferred Drug list is covered by MCPS.
CVS/Caremark updates the Primary Preferred
Drug list periodically, so you may need to work
with your doctor and Caremark to determine
which covered drug you will need to use in the
future. The complete list is available on the
CVS/Caremark website at www.caremark.com.
Compound Drug Preauthorization—Any
compound drug medication costing $300 or
more requires the doctor/pharmacist to receive
pre-authorization from Caremark before the
prescription is dispensed.
Morphine Milligram Equivalent (MME)
Based Limits—In response to the opioid
epidemic in the United States, CVS Caremark
has adopted use of the Morphine Milligram
Equivalent. MME is a calculation that converts
2024
EMPLOYEE BENEFIT SUMMARY
25
all opioids to the same units—a morphine
equivalent dose—so that the total amount of
opioids prescribed can be limited. The limits are
based on guidelines recently published by the
Centers for Disease Control (CDC). If a written
prescription exceeds the allowed limits,
physicians will need to contact CVS Health
Prior Authorization department at 1-800-294-
5979.
CVS Retail Pharmacy or CVS/Caremark
Mail Service Pharmacy—If you are taking a
maintenance medication, you are allowed an
initial fill and one refill up to a 30-day supply at
a retail pharmacy at the applicable copay.
Thereafter, you either must use the
CVS/Caremark Mail Service Pharmacy or fill
your maintenance medication prescription at any
CVS pharmacy. If you choose to purchase a
maintenance medication at a retail pharmacy
other than a CVS pharmacy after a second fill,
you will be required to pay the retail copay plus
the difference between the mail order and retail
cost of the drug.
To receive a 90-day supply of medication at a
CVS pharmacy, ask your doctor for a
prescription for up to a 90-day supply of
medication, plus refills as appropriate (three
refills maximum), and submit directly to the
CVS pharmacist.
To participate in the CVS/Caremark Mail
Service pharmacy, ask your doctor for a
prescription for up to a 90-day supply of
medication, plus refills as appropriate (three
refills maximum). Complete a Patient
Profile/Order Form, available from ERSC and
on the ERSC website, and mail the form, along
with the original prescription, to CVS/Caremark.
Keep a copy of the prescription for your records
and allow a minimum of 10 to 14 business days
for delivery. You can also order medications
online at www.caremark.com.
If you wish to change your current long-term
prescription from CVS/Caremark Mail Service
to a CVS pharmacy, you must call Customer
Care at 1-800-378-7558.
CVS/Caremark’s website provides information
on how to use the mail order benefit, forms you
can download (mail order claim, etc.), and a
feature to request refills once you are registered.
You also may obtain forms from ERSC and on
the ERSC website. You may choose to refill
your prescriptions using CVS/Caremark’s
automated telephone service at 1-800-378-7558.
If you fill a prescription at a non-participating
pharmacy, you must pay the full cost of the
prescription and may file a paper claim for
partial reimbursement. Reimbursement is limited
to the network price (an amount that is normally
less than the retail price) of the drug minus the
appropriate copay. Most major pharmacies
participate in the CVS/Caremark network.
Please ask your pharmacist or refer to the
CVS/Caremark website to determine if your
pharmacy participates with CVS/Caremark.
Diabetic Supplies—CVS/Caremark will cover
diabetic supplies, including test strips, lancets,
swabs, and meters. The medical plans will cover
Insulin Pumps and supplies associated with the
pumps under durable medical equipment
provisions. Supplies are limited up to the
following:
200 strips every 30 days
200 lancets every 30 days
200 alcohol swabs every 30 days
Lancet device limit of 1 per 180 days
You can receive up to 600 strips, swabs, and
lancets every 90 days either through a CVS
pharmacy or through the CVS/Caremark Mail
Service pharmacy. Diabetic supplies are
considered a maintenance drug and, therefore,
follow maintenance drug requirements.

2024
EMPLOYEE BENEFIT SUMMARY
26
Kaiser Permanente Prescription Plan
If you are enrolled in the Kaiser Permanente
HMO and elect to receive prescription drug
coverage, you will receive your coverage
through Kaiser Permanente.
The Kaiser plan pays for prescriptions you fill at
either Kaiser Medical Center pharmacies,
participating Kaiser network pharmacies, or
through Kaiser mail order pharmacy.
Short-term medications are those prescribed for
illnesses such as colds, flu, and ear/sinus
infections. You can obtain up to a 60-day supply
at a Kaiser Medical Center pharmacy or a Kaiser
participating network pharmacy.
Long-term maintenance medications and
prescriptions taken for chronic illnesses may be
obtained up to a 90-day supply via Kaiser’s mail
order program. Long-term maintenance
medications are those prescribed for high blood
pressure, arthritis, heart conditions, and diabetes.
The Kaiser plan does not pay benefits for over-
the-counter cosmetics, experimental drugs, or
vitamins. Prescriptions written by a dentist will
be covered when written either for antibiotics or
pain medications. For prescriptions that do not
meet these conditions, you must contact your
Kaiser physician; otherwise, you will not receive
benefits for these prescriptions.
Refer to the chart below for more information
about your costs for prescriptions under the plan.
Kaiser
Medical
Center
Pharmacy
(up to 60-day
supply)
Kaiser Network
Pharmacy (up
to 60-day
supply)
Mail Order
(up to 90-day
supply)
Kaiser
Generic
$10 copay $15 copay $15 copay
Kaiser
Brand
Name
(only when
no generic
equivalent
is available)
$10 copay $15 copay $20 copay
Retail Pharmacy—You can receive benefits for
prescriptions you fill at any participating Kaiser
Medical Center Pharmacy or any participating
Kaiser network pharmacy. Simply present your
Kaiser member ID card when you fill your
prescription. When you fill your prescription at a
Kaiser Medical Center Pharmacy, you pay the
$10 copay for up to a 60-day supply for a
generic drug or the $10 copay for up to a 60-day
supply of a brand name drug when there is not a
generic available. When you fill your
prescription at a participating Kaiser network
pharmacy, you can receive up to a 60-day supply
of a generic drug for a copay of $15 or up to a
60-day supply of a brand name drug for a $15
copay when there is not a generic available.
Major and independent pharmacies participate
with Kaiser. Please visit Kaiser’s website at
www.kp.org for a complete list. The quantity
limitation for medications obtained on the retail
level is up to a 60-day supply.
Mail Order Service—You can use the mail
order program to fill up to a 90-day supply of
maintenance medications with the $15 copay for
generic drugs or the $20 copay for brand name
drugs when there is not a generic available.
There is no cost for shipping. Refills can be
made online or through your Kaiser Permanente
app. You must be registered on kp.org.
Download and use the app, or order online. To
participate in the mail order program, ask your
doctor for a written prescription for up to a 90-
day supply of medication, plus refills as
appropriate. You should fill new maintenance
prescriptions at your Kaiser Medical Center
Pharmacy for the first fill so that you have the
opportunity to consult with a pharmacist. Allow
seven business days for delivery.
Insulin has the same coverage as other
prescription medications.
2024
EMPLOYEE BENEFIT SUMMARY
27
Life Insurance
EMPLOYEE LIFE INSURANCE
Basic Employee Term Life
Insurance
New employees who are eligible for benefits
automatically receive basic employee term life
insurance effective the first day of the month
following their hire date.* Term life insurance
has no cash value.
If you do not wish to participate in the basic
term life insurance program, you must decline
life insurance coverage when you enroll in
benefits online using the BES.
Once you decline coverage, you may enroll only
during the annual Open Enrollment by providing
evidence of insurability and receiving approval
from the insurer.
The amount of basic term life insurance you
receive is determined by rounding your annual
salary to the closest thousand dollars and
multiplying by two. Overtime, stipends, and
non-guaranteed supplemental earnings are not
included in this calculation.
For Example
An employee with a salary of $52,300 would have
$104,000 of employee basic term life insurance coverage
($52,000 times 2).
You and MCPS share the cost of your basic term
life insurance coverage. You pay 17 percent of
the cost for coverage and MCPS pays 83
percent. MCPS pays 100 percent of the cost for
basic dependent term life insurance.
Please remember to update your beneficiary
information as your personal situations change.
You can make beneficiary updates online during
Open Enrollment, or during the plan year by
completing the MCPS Form 455-20 Employee
Benefit Plan Enrollment. (Note: The enrollment
form does not update your beneficiaries for
retirement/pension plans or 403(b) or 457(b)
defined contribution plans.)
Accelerated Death Benefit—Your employee
life insurance plans offer an accelerated death
benefit. This benefit does not apply to dependent
life insurance plans. The accelerated death
benefit provides a payment of up to 80 percent
of your employee life insurance benefit if your
life expectancy is 12 months or less, and the
payment can be used for any purpose. Any
remaining life insurance benefits will be paid to
your beneficiary(ies) after your death.
To apply for this benefit, you and the attending
physician must complete and submit the two
accelerated death benefit claim forms, which are
available on the ERSC website. Please read the
instructions carefully and forward the completed
forms to ERSC.
*For 10-month employees reporting for the
school year in August, coverage begins
October 1.
Optional Employee Term Life
Insurance
If you are enrolled in basic employee term life
insurance, you also may choose to purchase
additional life insurance equal to one times your
annual salary (rounded down to the nearest
thousand). Employee cost for optional life
insurance coverage is outlined in the life
insurance rate chart which appears later in this
document.
The cost of optional employee life insurance is
based on your age, and you pay the full cost of
coverage through payroll deduction. New
employees are not required to submit evidence
of insurability when selecting coverage,
provided they enroll within 60 days of
employment via the online BES.
If you did not elect coverage during your initial
period of eligibility, you are required to provide
evidence of insurability and be approved for
coverage by the insurer when you enroll during
the next annual Open Enrollment.

2024
EMPLOYEE BENEFIT SUMMARY
28
DEPENDENT TERM LIFE INSURANCE
Benefits-eligible employees who are enrolled in
basic employee term life insurance also may
choose two levels of life insurance for their
eligible dependents: basic dependent life
insurance and optional dependent life insurance.
You are always the beneficiary for dependent
life insurance.
If your spouse also is employed by MCPS,
neither of you may elect dependent life
insurance for his/her spouse.
Children no longer are eligible for dependent
basic and/or optional life insurance as of
September 30 following their 23rd birthday.
Employees must notify ERSC when a child
reaches age 23 so that they may be removed
from this coverage and deductions reduced
appropriately.
Under IRS regulations, you are taxed on the
value of the employer-paid portion of premiums
for all coverage in excess of $50,000. This
taxable imputed income appears on your
ePaystub as EXS Life.
Basic Dependent Term Life Insurance
If you are enrolled in basic employee term life
insurance, you automatically receive dependent
life insurance coverage for your spouse and any
eligible dependent children at no additional cost
as follows:
$2,000 for your eligible spouse, and
$1,000 for each eligible dependent child.
Optional Dependent Term Life
Insurance
If you are enrolled for basic dependent life
insurance, you may choose to purchase
additional dependent life insurance in the
amount of $10,000 for each eligible dependent.
The cost of coverage is based on a flat rate,
regardless of the number of dependents you
enroll. You pay for the full cost of this coverage.
This coverage includes your spouse and any
eligible dependent child. If your spouse also is
employed by MCPS, you may not elect
dependent life insurance for him/her.
Otherwise, you must wait until the next annual
Open Enrollment to enroll your dependents.
Dependents age 19 or older will be required to
provide evidence of insurability and be approved
for coverage by the insurer.
If you have a qualifying event, such as marriage
or birth of a child, you must complete MCPS
Form 450-2 Optional Employee Term Life
Insurance Enrollment/Cancellation, within 60
days of the event to enroll your dependents in
optional dependent life, or elect to enroll in the
Optional Dependent Life coverage through the
Benefit Enrollment System.
In the event of the death of an eligible
dependent, employees should notify ERSC by
email or phone. Claim forms will then be
provided in order to process the claim with the
life insurance vendor.
Flexible Spending
Accounts
Flexible Spending Accounts (FSAs) provide you
with a tax-saving opportunity. The plan year
begins January 1 of the current year and
continues through March 15 of the following
year. The plan year determines the period of
time you may incur expenses. The calendar year
begins January 1 of the current year and
continues through December 31 of the current
year. The calendar year determines the period of
time you make contributions. Under the FSA
plan, you may set aside a portion of your salary
before taxes are deducted to pay for anticipated,
qualifying expenses such as day care for a child
under age 13 or medical expenses not covered
by an insurance plan. You have two FSA plan
options:
Dependent Care Account—Set aside up to a
combined family maximum of $5,000/year,
or $2,500/year if filing separately, from your
salary to pay for qualified dependent care
2024
EMPLOYEE BENEFIT SUMMARY
29
expenses. Qualified dependent care
expenses are expenses incurred for the care
of children under age 13 or disabled
dependents while you are working, disabled,
or attending school. Qualified expenses
include day care, nursery school, summer
day camps, and in-home care.
Medical Spending Account—Set aside up to
$3,050 from your salary per calendar year to
pay for qualified medical expenses.
Qualified expenses include deductibles,
copayments, expenses in excess of plan
limits, and qualified costs not covered by
any benefit plan. Cosmetic procedures are
not qualified expenses under a medical
spending account.
Benefit Strategies administers MCPS flexible
spending accounts. Visit the Benefit Strategies
website at https://benstrat.navigatorsuite.com
for a complete
listing o
f eligible expenses for
dependent care and med
ical spending accounts.
You are eligible to enroll in the FSA plan if you
are a permanent employee working at least 20
hours a week, even if you do not participate in
health coverage through MCPS.
When you are newly hired, you have 60 days
from your date of hire to enroll in the FSA plan
via the BES. After that time, you may only
enroll for the FSA plan online during the annual
Open Enrollment, unless you have a qualifying
event. If you experience a qualifying event, you
have 60 days from the date of the event to enroll
in the FSA plan using the BES. Qualifying
events include marriage or divorce, addition or
loss of a dependent, spouse becomes eligible for
or loses medical coverage, spouse loses full-time
employment or you return from leave.
You may enroll in one or both accounts subject
to a $100 annual minimum per account.
Elections are made one year at a time and do not
carry forward from year-to-year. If you wish to
participate, you must make a new FSA election
each year during Open Enrollment.
You decide how much to contribute to your FSA
plan on a calendar year basis. The amount you
specify will be withheld from your paycheck in
equal amounts on a pretax basis. When you
incur a qualified expense for dependent care,
you file a claim for reimbursement from your
FSA plan through Benefit Strategies. Then, you
are reimbursed from your FSA plan with pretax
dollars.
When you contribute to a medical and/or
dependent care FSA, you will receive a
Mastercard debit card that is good for three
consecutive years if you reenroll each
calendar year. Using the Mastercard debit card
provides immediate access to the funds in your
FSA. You can use the debit card to cover the
costs of certain eligible health and dependent
care services so you do not have to file a claim
for reimbursement.
Be sure to visit the following website to create
an account with Benefit Strategies so you can
submit claims and track expenses:
https://benstrat.navigatorsuite.com
Important Reminder to Mastercard Debit
Card Users
All expenditures are subject to audit. It is important to retain
all receipts.
You are not required to use the Mastercard debit
card for reimbursement of eligible expenses. If
you prefer, you can submit a paper claim along
with receipts for eligible expenses directly to
Benefit Strategies for reimbursement.
When submitting for reimbursement using a
claim form, mail or fax the form, Explanation of
Benefits (EOB), billing statement showing the
service provided, and receipt(s), to Benefit
Strategies. You will be reimbursed for all
eligible expenses not covered by your health
plan. You can sign up for direct deposit at
https://benstrat.navigatorsuite.com.
There are separate reimbursement forms for the
medical and dependent care accounts.
Reimbursement forms are available on the
ERSC website. IRS regulations do not permit
FSA election changes during the year unless a
qualifying event such as marriage, divorce,

2024
EMPLOYEE BENEFIT SUMMARY
30
addition or loss of a dependent, or change of
employment status occurs.
IRS regulations impose a “use or lose” rule due
to the tax advantages of the FSA plan. This rule
requires that any money not used by the end of
the plan year is forfeited. In addition, you are not
permitted to transfer funds from one account to
the other. It is very important to fully understand
the program and carefully estimate qualifying
expenses before enrolling.
An IRS regulation provides plan participants
enrolled in the medical and dependent care FSA
with an additional two and one-half months to
incur claims for the plan year. Qualifying
medical and/or dependent care expenses
incurred from January 1, 2024, through March
15, 2025, may be reimbursed from funds set
aside for the 2024 calendar year.
If there is a balance in the 2024 plan year
account, qualifying expenses incurred between
January 1, 2025, and March 15, 2025, may be
reimbursed from either the 2024 or 2025 plan
year account (but not from both plan years). All
claim requests for reimbursement of expenses
incurred during the 2024 plan year must be
submitted and received by Benefit Strategies no
later than April 30, 2025.
To be considered, appeals for FSA accounts
must be received within 90 days following April
30—the claim filing deadline.
You cannot continue your participation in the
flexible spending accounts (FSAs) while on
leave. Your FSAs are cancelled as of the last
deduction taken once you are on leave. You
must reenroll within 60 days of returning from
leave. You can incur expenses up to the date
your leave begins and have until April 30
following the plan year to submit claims for
reimbursement.
Please note: Returning from leave is not a
qualifying event to change your election amount.
Employees who begin leave, terminate
employment, or retire will be reimbursed for
qualified expenses incurred prior to beginning
leave and/or separation of employment with
MCPS, and they must submit claim receipts for
reimbursement by April 30 following the plan
year. Expenses incurred after you begin leave,
terminate employment, or retire are not qualified
expenses.
Additional information, estimation worksheets,
and reimbursement forms are available on the
ERSC website.
403(b) Tax Sheltered
Savings and
457(b) Deferred
Compensation Plans
(Defined Contribution Plans)
MCPS offers two voluntary defined contribution
plans to all employees:
403(b) Tax Sheltered Savings Plan
457(b) Deferred Compensation Plan
The plan
s offer a means to supplement your
retirement savings while reducing current
taxable income. You can choose to participate in
the 403(
b) plan, the 457(b) plan, or both plans.
You decide how much of your salary to
contribute to an account in your name
administered by Fidelity Investments.
Contributions from your salary are made on a
pretax basis through payroll deductions. The
contributions are then invested in investment
options that you have selected from the MCPS
investment menu. You will pay income taxes on
your contributions and any investment earnings
when you withdraw money from your account.
You may begin participating in the Fidelity
403(b) and/or 457(b) plan(s) at any time. You
can also change or stop the amount you are
contributing to your 403(b)/457(b) account(s) at
any time. To start an account or to modify your
contribution, log in to www.netbenefits.com/mcps
or contact Fidelity at 1-800-343-0860. Please
allow one to two pay periods for your changes to
be effective. If you have any questions about
2024
EMPLOYEE BENEFIT SUMMARY
31
your 403(b) and/or 457(b) plan(s), please contact
Fidelity at 1-800-343-0860.
The rules and regulations of the plans are
governed by IRS rules and the plan documents.
For example, the total amount you may
contribute in a calendar year is determined by
limits set by the IRS. Please keep in mind the
funds in your 403(b) and/or 457(b) accounts are
intended for retirement, and you may not have
penalty-free access to the funds until you meet
one of the withdrawal requirements such as a
certain age or separation of service. You may
visit www.irs.gov and www.netbenefits.com/mcps
for more information.
Applying for Distribution of Funds
from 403(b) and/or 457(b) Accounts
After Retirement
Participants enrolled in a 403(b) plan may begin
withdrawals at age 59½ while still employed. If
you have a 403(b), IRS penalties will apply if
you separate from service and make withdrawals
before age 59 ½. There are exceptions. Consult
www.irs.gov for further information.
If you have a 457(b), you may begin penalty-
free withdrawals at age 59½ while still
employed or upon separation from service at any
age. If 403(b) and/or 457(b) plan participants
separate from service and then become re-
employed by MCPS in any capacity, penalty-
free withdrawals are not permitted if they are
under age 59½.
403(b) and/or 457(b) benefits are taxable in the
year of withdrawal. The IRS generally requires
that you start taking withdrawals, Required
Minimum Distributions (RMDs), from your
403(b) and/or 457(b) account(s) when you reach
age 73 (72 if you turned 72 in 2022 or earlier;
70½ if you turned 70½ in 2019 or earlier) or
retire. To request your withdrawal from Fidelity
Investments, contact a Fidelity representative at
1-800-343-0860. If you have questions about the
withdrawal process at another vendor, please
contact that vendor directly. Contact information
for previous vendors is available at
www.netbenefits.com/mcps.
Important
As a plan participant, you are responsible for the review and
selection of any and all investment options. You must review
them carefully before making any investment decisions.
Neither MCPS nor any of its employees has any liability or
responsibility for investment options that you select.
Well Aware: Employee
Wellness Program
MCPS offers the Well Aware employee wellness
program to all benefits-eligible employees free of
charge. Well Aware’s mission is to establish a
work environment that promotes healthy
lifestyles, decreases the risk of disease, enhances
quality of life, and recognizes employee health
and wellness as a cultural priority in the long-
term success of MCPS as a whole. This program
encourages strengthening health and well-being
through convenient access to educational
opportunities, wellness activities, behavioral
change programs, and awareness events.
Well Aware supports employees in their efforts
to lead healthy lifestyles by providing discounts
on health and wellbeing services, a smoking
cessation program, activity challenges, and
educational outreach. To learn more about Well
Aware and to view a calendar of upcoming
wellness events, visit the Well Aware web page
by searching for “staff wellness” from any
MCPS web page or go to
https://www2.montgomeryschoolsmd.org/staff/
wellness/.

2024
EMPLOYEE BENEFIT SUMMARY
32
Retirement Benefits
SOCIAL SECURITY
As an MCPS employee, you pay Social Security
and Medicare taxes on your earnings and are
eligible to qualify for benefits under the Social
Security program. If you earn 40 credits (10
years of work) under the program, you will
qualify for a future Social Security retirement
benefit.
“Social Security: Understanding the Benefits”
(Publication No. 05-10024) provides a summary
of the Social Security program and includes
instructions on estimating your Social Security
retirement benefit. The summary is available
free of charge from the Social Security
Administration by calling 1-800-772-1213 or by
visiting their website at www.ssa.gov/.
PENSION PLANS
MCPS offers comprehensive retirement benefits,
including pension plans, to its retired employees.
For details, please see Understanding Your
Retirement, which is available online at
www.montgomeryschoolsmd.org/uploadedFiles/
departments/ersc/employees/retirement-
planning/understanding_your_retirement.pdf.
POSTRETIREMENT HEALTH
BENEFITS
MCPS employees who meet eligibility
requirements may obtain health insurance
benefits in retirement. As an active employee
who may be eligible for retirement at the time of
their death, the surviving spouse will be required
to elect the Spousal continuation pension option
in order to remain eligible for MCPS health
benefits.
Eligibility rules and cost share details are
included in the Retiree Benefit Summary
available at
www.montgomeryschoolsmd.org/uploadedFiles/
retiree_benefit_summary_current.pdf.
WELLNESS INITIATIVES IN
RETIREMENT
When you retire, any Wellness Initiatives
program credits you earned as an active
employee will not carry over into retirement. A
retiring employee needs to complete their
biometric health screening and health risk
assessment again, as a retiree, to receive the
credits for the following benefit plan year.
Ten-month employees who retire on July 1
and whose retiree benefits do not begin until
October 1 will have from October 1
of the
current year until the Friday before Open
Enrollment begins that year to complete their
biometric health screening and health risk
assessment as a retiree.
Wellness Initiatives credits no longer apply if the
retiring employee is Medicare-eligible at the time
of retirement.
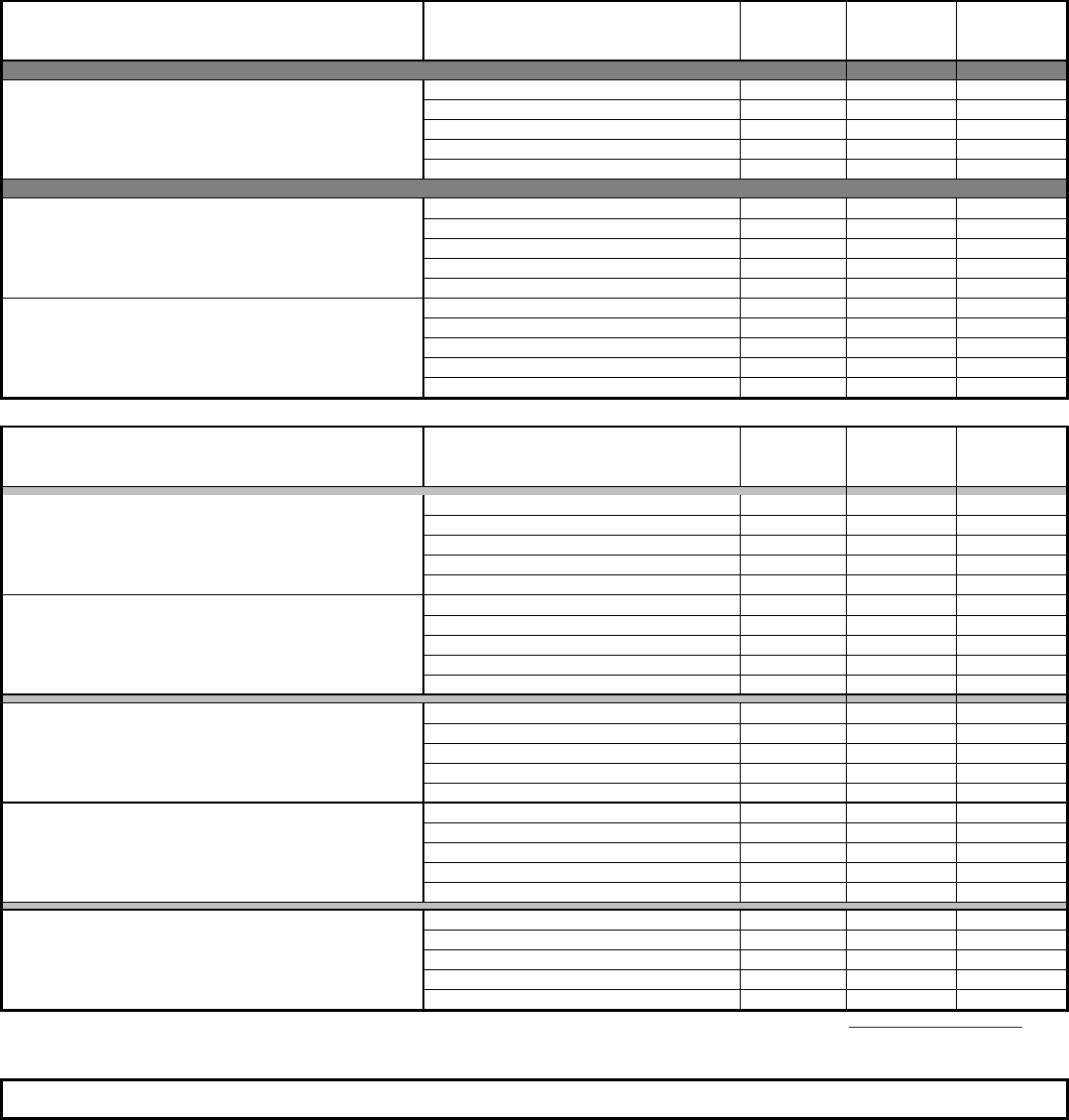
Active Employee Cost - Calendar Year 2024
Healthcare Costs
Completed Neither Health Risk Assessment nor Biometric Health Screening
Base Employee Cost Share*
Effective January 1, 2024
Medical Plans
Coverage Level
Employee
Percentage
Biweekly
10-Month
Employee
Biweekly
12-Month
Employee
Point of Service Plans
Cigna POS Individual 17% 71.48 54.99
Individual + Spouse 17% 142.96 109.97
Individual + Child 17% 142.96 109.97
Family (Individual + Spouse + Child(ren)) 17% 194.52 149.63
Family (Individual + Children) 17% 194.52 149.63
Health Maintenance Organization Plans
Cigna HMO Individual 12% 35.54 27.34
Individual + Spouse 12% 66.79 51.38
Individual + Child 12% 66.79 51.38
Family (Individual + Spouse + Child(ren)) 12% 109.43 84.18
Family (Individual + Children) 12% 109.43 84.18
Kaiser Permanente HMO Individual 12% 46.97 36.13
Individual + Spouse 12% 93.75 72.12
Individual + Child 12% 93.75 72.12
Family (Individual + Spouse + Child(ren)) 12% 135.85 104.50
Family (Individual + Children) 12% 135.85 104.50
Supplemental Plans
Coverage Level
Employee
Percentage
Biweekly
10-Month
Employee
Biweekly
12-Month
Employee
Caremark Prescription Individual 17% 19.72 15.17
Individual + Spouse 17% 39.40 30.31
Individual + Child 17% 39.40 30.31
Family (Individual + Spouse + Child(ren)) 17% 48.62 37.40
Family (Individual + Children) 17% 48.62 37.40
Kaiser Permanente Prescription Individual 17% 8.58 6.60
Individual + Spouse 17% 17.00 13.08
Individual + Child 17% 17.00 13.08
Family (Individual + Spouse + Child(ren)) 17% 24.57 18.90
Family (Individual + Children) 17% 24.57 18.90
CareFirst Dental PPO Individual 17% 3.65 2.81
Individual + Spouse 17% 7.30 5.62
Individual + Child 17% 7.30 5.62
Family (Individual + Spouse + Child(ren)) 17% 10.73 8.25
Family (Individual + Children) 17% 10.73 8.25
Aetna Dental DMO Individual 17% 2.20 1.69
Individual + Spouse 17% 4.40 3.38
Individual + Child 17% 4.40 3.38
Family (Individual + Spouse + Child(ren)) 17% 6.46 4.97
Family (Individual + Children) 17% 6.46 4.97
Davis Vision Individual 17% 0.19 0.14
Individual + Spouse 17% 0.34 0.26
Individual + Child 17% 0.34 0.26
Family (Individual + Spouse + Child(ren)) 17% 0.43 0.33
Family (Individual + Children) 17% 0.43 0.33
*Your rates may vary based on your participation in the Wellness Initiatives program. Visit the Employee Benefits web page to see all of the rate combinations.
Employee Benefits web page
Employee Life Insurance 100% rate = $.068 per thousand of insurance per month
Based on two times current salary rounded to the nearest $1,000
33
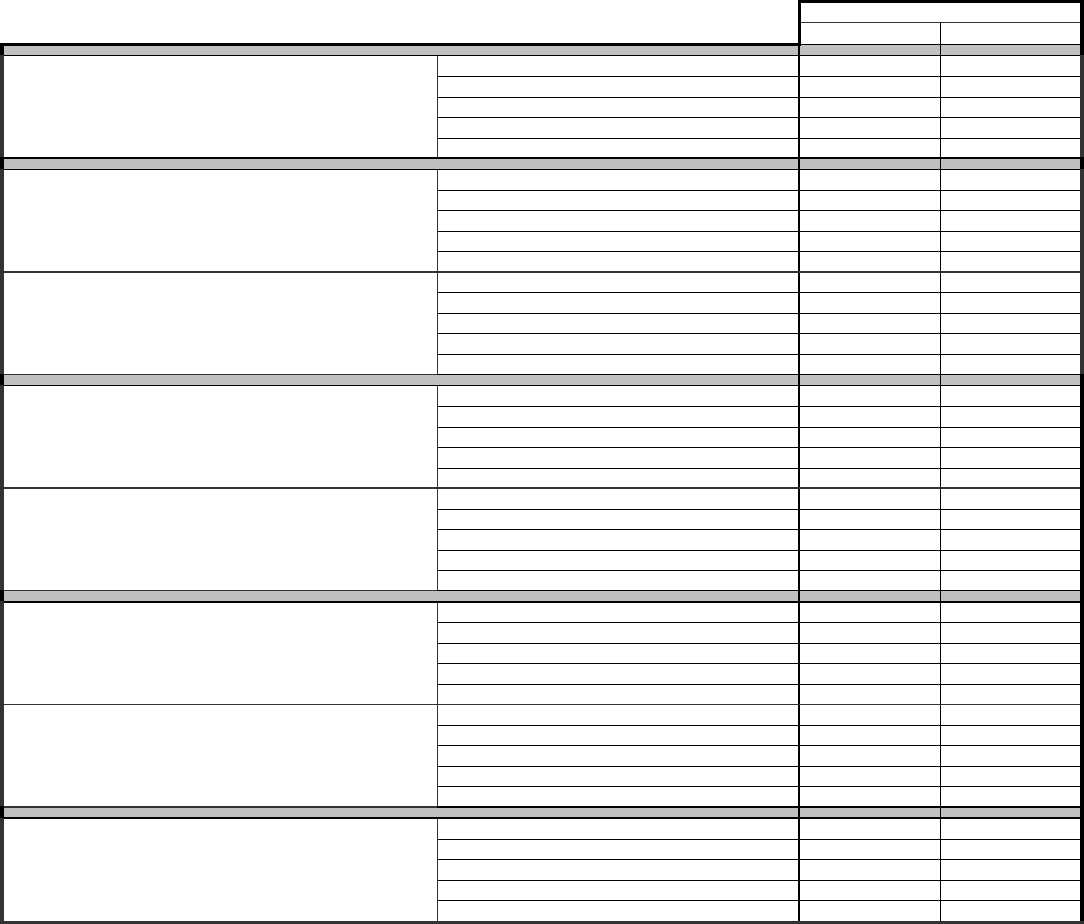
Active Employee Cost - Calendar Year 2024
LEAVE RATE SCHEDULE
100% ACTIVE EMPLOYEE RATE
Effective January 1, 2024
Component Cost
MONTHLY ANNUAL
Cigna POS Individual 700.81 8,409.72
Individual + Spouse 1,401.58 16,818.96
Individual + Child 1,401.58 16,818.96
Family (Individual + Spouse + Child(ren)) 1,907.03 22,884.36
Family (Individual + Children) 1,907.03 22,884.36
Cigna HMO Individual 493.55 5,922.60
Individual + Spouse 927.65 11,131.80
Individual + Child 927.65 11,131.80
Family (Individual + Spouse + Child(ren)) 1,519.80 18,237.60
Family (Individual + Children) 1,519.80 18,237.60
Kaiser Permanente HMO Individual 652.45 7,829.40
Individual + Spouse 1,302.09 15,625.08
Individual + Child 1,302.09 15,625.08
Family (Individual + Spouse + Child(ren)) 1,886.75 22,641.00
Family (Individual + Children) 1,886.75 22,641.00
Caremark Prescription Individual 193.35 2,320.20
Individual + Spouse 386.30 4,635.60
Individual + Child 386.30 4,635.60
Family (Individual + Spouse + Child(ren)) 476.70 5,720.40
Family (Individual + Children) 476.70 5,720.40
Kaiser Permanente Prescription Individual 84.10 1,009.20
Individual + Spouse 166.60 1,999.20
Individual + Child 166.60 1,999.20
Family (Individual + Spouse + Child(ren)) 240.84 2,890.08
Family (Individual + Children) 240.84 2,890.08
CareFirst PPO Dental Individual 35.76 429.12
Individual + Spouse 71.56 858.72
Individual + Child 71.56 858.72
Family (Individual + Spouse + Child(ren)) 105.12 1,261.44
Family (Individual + Children) 105.12 1,261.44
Aetna DMO Dental Individual 21.55 258.60
Individual + Spouse 43.12 517.44
Individual + Child 43.12 517.44
Family (Individual + Spouse + Child(ren)) 63.28 759.36
Family (Individual + Children) 63.28 759.36
Davis Vision Individual 1.85 22.20
Individual + Spouse 3.40 40.80
Individual + Child 3.40 40.80
Family (Individual + Spouse + Child(ren)) 4.31 51.72
Family (Individual + Children) 4.31 51.72
34
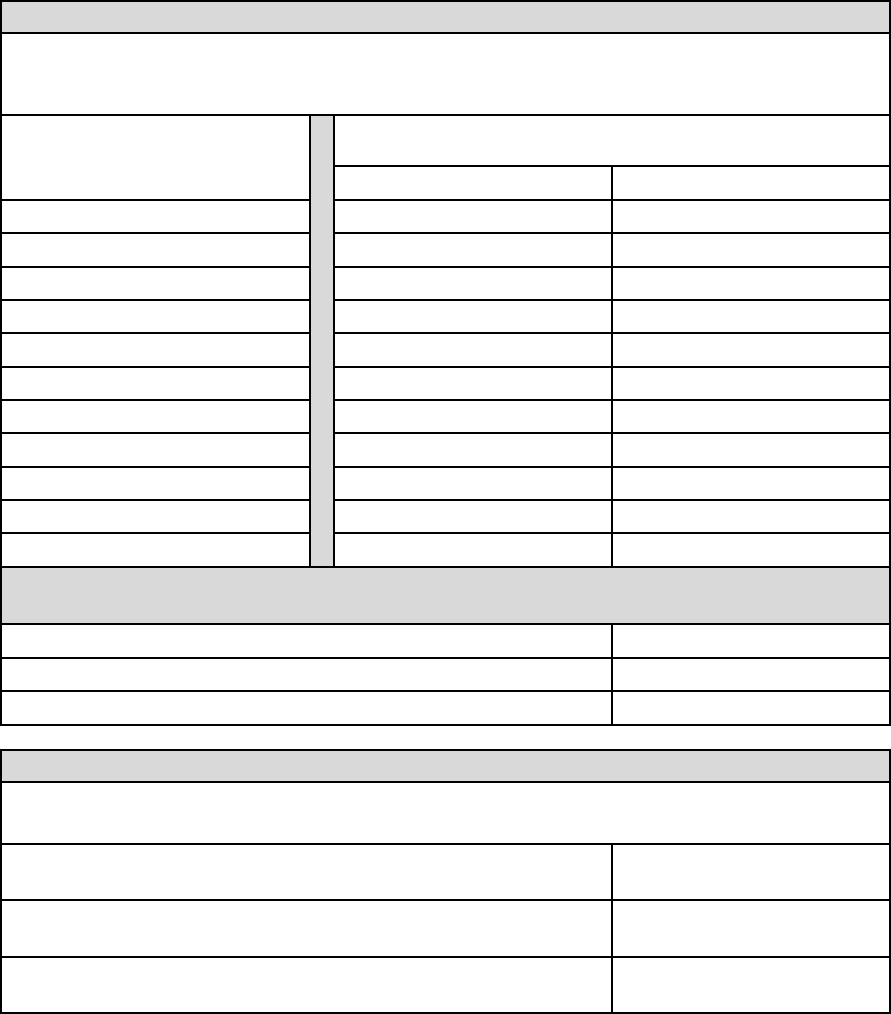
Active Employee Cost - Calendar Year 2024
Optional Term Life Insurance (Employee and Dependent)
Effective January 1, 2024
10-month 12-month
Under 25 0.014 0.011
25 - 29 0.017 0.013
30 - 34 0.019 0.015
35 - 39 0.023 0.018
40 - 44 0.026 0.020
45 - 49 0.040 0.031
50 - 54 0.057 0.044
55 - 59 0.111 0.085
60 - 64 0.168 0.129
65 - 69 0.325 0.250
70 and over 0.530 0.408
$46,000.00
46
$1.06
$10,000.00
$1.15
$1.50
Bi-weekly payroll deduction for 12-month employees
Bi-weekly payroll deduction for 10-month employees
Coverage Amount (one times the annual salary)
Thousands of Coverage
Bi-weekly Cost = 46 x .023
Optional Dependent Term Life Insurance
You must be enrolled in Basic Employee Term Life coverage to elect Optional Dependent Term Life coverage. Coverage
for qualified dependent children will continue until September 30 following their 23
rd
birthday.
Coverage Amount for each qualified dependent spouse and/or
dependent child(ren)
Optional Employee Term Life Insurance
Eligible employees enrolled for basic term life insurance are entitled to purchase additonal one times their salary (rounded
down to the nearest thousand) in life insurance. The cost of optional life insurance is based on age and is paid entirely by
the employee through payroll deductions.
Age Bracket
Bi-weekly Employee Deductions
(per thousand of coverage)
SAMPLE CALCULATION: Optional Term Life Insurance Coverage rates for a 37 year-old, 10-month
employee who earns $46,000 a year.
35

2024
EMPLOYEE BENEFIT SUMMARY
36
Websites an
d
Tele
p
hone Numbers
Employee and Retiree Service Cent
er
30
1-517-8100
www.montgomeryschoolsmd.org/departments/ersc
MCPS Help Desk (to reset MCPS ID/password)
301-517-5800
Office of Human Resources and Development
301-279-3204
www.montgomeryschoolsmd.org/departments/
personnel
Aetna Dental Plan (DMO)
1-800-843-3661
www.aetna.com
American Fidelity
1-800-662-1113
https://americanfidelity.com/
Benefit Strategies COBRA
1-888-401-3539
www.benstrat.com
Benefit Strategies Flexible Spending Accounts
1-888-401-3539
https://benstrat.navigatorsuite.com
Cigna Open Access Plus POS Plan
Cigna Open Access Plus In-Network HMO Plan
Cigna Indemnity Plan
1-800-Cigna24
www.MyCigna.com
CareFirst Preferred Dental (PPO)
In-network: 1-888-755-2657
www.carefirst.com/mcps
CVS Caremark Prescription Plan
1-800-378-7558
www.caremark.com
Davis Vision/Blue Vision Plus
(provided through Ca
reFirst)
1-800-783-5602
www.carefirst.com/mcps
Kaiser Permanente HMO and
Prescription Plans
1-800-777-7902
www.kp.org
Maryland State Retirement Agency
1-800-492-5909
https://sra.maryland.gov/
Maryland State Retirement Agency—
Local Member Services
410-625-5555
MCAAP (Administrators Union)
301-762-8174
MCBOA (Non-certified Supervisors Union)
301-762-8174
MCEA (Teachers Union)
301-294-6232
www.mceanea.org
MCPS 403(b)/457(b) Plans
Fidelity Investments
1-800-343-0860
www.netbenefits.com/mcps
MetLife
1-800-638-6420
www.metlife.com/mybenefits
SEIU Local 500
301-740-7100
www.seiu500.org
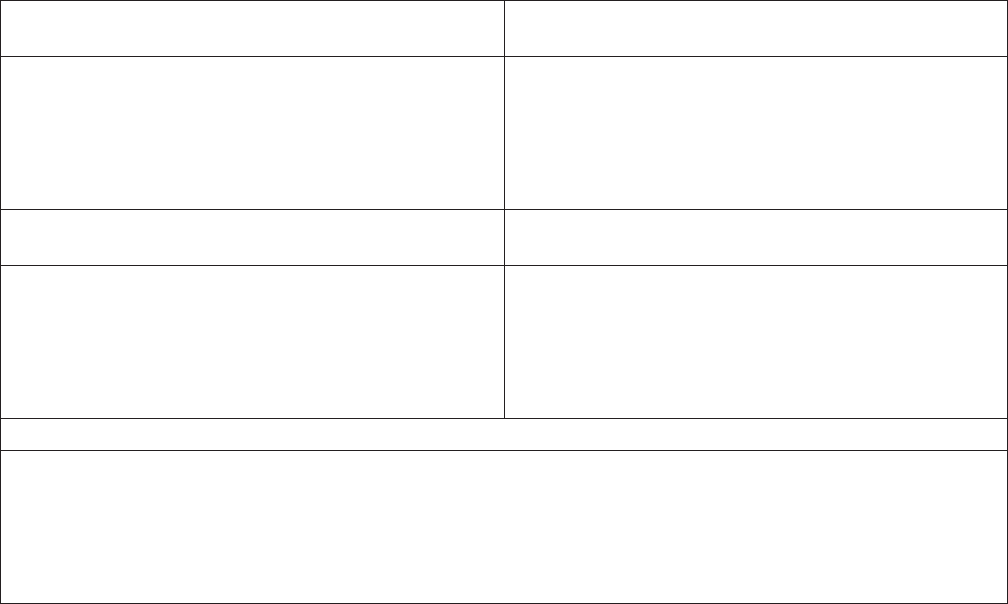
VISION
We inspire learning by
providing the greatest
public education to each
and every student.
MISSION
Every student will have
the academic, creative
problem solving, and
social emotional skills
to be successful in
college and career.
CORE PURPOSE
Prepare all students to
thrive in their future.
CORE VALUES
Learning
Relationships
Respect
Excellence
Equity
Board of Education
Ms. Karla Silvestre
President
Mrs. Shebra L. Evans
Vice President
Ms. Lynne Harris
Ms. Grace Rivera-Oven
Mrs. Rebecca K. Smondrowski
Ms. Brenda Wolff
Ms. Julie Yang
Mr. Sami Saeed
Student Member
Montgomery County Public Schools (MCPS)
Administration
Monifa B. McKnight, Ed.D.
Superintendent of Schools
Mr. M. Brian Hull
Chief Operating Officer
Patrick K. Murphy, Ed.D.
Deputy Superintendent
Mr. Brian S. Stockton
Chief of Staff
Mrs. Stephanie P. Williams
General Counsel
Ms. Elba M. Garcia
Senior Community Advisor
Dr. Patricia E. Kapunan
School System Medical Officer
850 Hungerford Drive
Rockville, Maryland 20850
www.montgomeryschoolsmd.org
MCPS NONDISCRIMINATION STATEMENT
Montgomery County Public Schools (MCPS) prohibits illegal discrimination based on race, ethnicity, color, ancestry, national origin,
nationality, religion, immigration status, sex, gender, gender identity, gender expression, sexual orientation, family structure/
parental status, marital status, age, ability (cognitive, social/emotional, and physical), poverty and socioeconomic status,
language, or other legally or constitutionally protected attributes or affiliations. Discrimination undermines our community’s
long-standing efforts to create, foster, and promote equity, inclusion, and acceptance for all. The Board prohibits the use of
language and/or the display of images and symbols that promote hate and can be reasonably expected to cause substantial
disruption to school or district operations or activities. For more information, please review Montgomery County Board of
Education Policy ACA, Nondiscrimination, Equity, and Cultural Proficiency. This Policy affirms the Board’s belief that each and every
student matters, and in particular, that educational outcomes should never be predictable by any individual’s actual or perceived
personal characteristics. The Policy also recognizes that equity requires proactive steps to identify and redress implicit biases,
practices that have an unjustified disparate impact, and structural and institutional barriers that impede equality of educational
or employment opportunities. MCPS also provides equal access to the Boy/Girl Scouts and other designated youth groups.**
For inquiries or complaints about discrimination against
MCPS students*
For inquiries or complaints about discrimination against
MCPS staff*
Director of Student Welfare and Compliance
Office of District Operations
Student Welfare and Compliance
850 Hungerford Drive, Room 55, Rockville, MD 20850
240-740-3215
SWC@mcpsmd.org
Human Resource Compliance Officer
Office of Human Resources and Development
Department of Compliance and Investigations
45 West Gude Drive, Suite 2500, Rockville, MD 20850
240-740-2888
For student requests for accommodations under
Section 504 of the Rehabilitation Act of 1973
For staff requests for accommodations under
the Americans with Disabilities Act
Section 504 Coordinator
Office of School Support and Well-being
Office of Well-being, Learning and Achievement
850 Hungerford Drive, Room 257, Rockville, MD 20850
240-740-5630
504@mcpsmd.org
ADA Compliance Coordinator
Office of Human Resources and Development
Department of Compliance and Investigations
45 West Gude Drive, Suite 2500, Rockville, MD 20850
240-740-2888
For inquiries or complaints about sex discrimination under Title IX, including sexual harassment, against students or staff*
Title IX Coordinator
Office of District Operations
Student Welfare and Compliance
850 Hungerford Drive, Room 55, Rockville, MD 20850
240-740-3215
TitleI[email protected]
* Discrimination complaints may be filed with other agencies, such as the following: U.S. Equal Employment Opportunity Commission (EEOC),
Baltimore Field Office, GH Fallon Federal Building, 31 Hopkins Plaza, Suite 1432, Baltimore, MD 21201, 1-800-669-4000, 1-800-669-
6820 (TTY); Maryland Commission on Civil Rights (MCCR), William Donald Schaefer Tower, 6 Saint Paul Street, Suite 900, Baltimore, MD
21202, 410-767-8600, 1-800-637-6247, mccr@maryland.gov; or U.S. Department of Education, Office for Civil Rights (OCR), The Wanamaker
Building, 100 Penn Square East, Suite 515, Philadelphia, PA 19107, 1-800-421-3481, 1-800-877-8339 (TDD), OCR@ed.gov, or www2.ed.gov/
about/offices/list/ocr/complaintintro.html.
**This notification complies with the federal Elementary and Secondary Education Act, as amended.
This document is available, upon request, in languages other than English and in an alternate format under the Americans with Disabilities
Act, by contacting the MCPS Office of Communications at 240-740-2837, 1-800-735-2258 (Maryland Relay), or PIO@mcpsmd.org.
Individuals who need sign language interpretation or cued speech transliteration may contact the MCPS Office of Interpreting Services
at 240-740-1800, 301-637-2958 (VP) mcpsinterpretingservices@mcpsmd.org, or MCPSInterpretingServices@mcpsmd.org.
July 2023
Published by the Department of Materials Management for the Employee and Retiree Service Center
0218.24 • Editorial, Graphics & Publishing Services • 9.23 • 1,500
Copyright
©
2023 Montgomery County Public Schools
