FEHB
Federal Employees
Health Benefits
Federal Employees
Health Benefits
(FEHB)
Facts
Program.
Information for Federal Civilian
Employees on the
Federal Employees Health Benefits
United States Office of
Retirement And Insurance Service
Personnel Management
RI 75-13
January 2001
Table of Contents
Page
What Is the Federal Employees Health Benefits (FEHB) Program? ...........1
When Can I Change From a Self and Family Enrollment To a Self Only
Can My Former Spouse Continue Federal Employees Health Benefits
Can Someone Be Covered Under More Than One Federal Employees Health
Can I Enroll? ....................................1
Do I Have to Join? .................................1
What Does the Federal Employees Health Benefits (FEHB) Program Offer?. . . 2
How Do I Stay Informed About FEHB and Participating Health Plans? .....2
Do I Pay for Federal Employees Health Benefits (FEHB) Coverage?.......3
What Is Premium Conversion? ...........................3
What Types of Plans Are Available?........................5
Fee-for-Service Plans .............................5
Health Maintenance Organizations (HMOs) .................6
Point of Service ................................7
What Types of Enrollment Are Available? ....................7
Self Only ...................................7
Self and Family ................................7
Which Family Members Are Covered Under My Enrollment? ..........8
When Does My Family Member Lose Coverage? .................9
Enrollment?.....................................9
(FEHB) Coverage? ................................10
Benefits (FEHB) Enrollment? ..........................11
i
When Can I Enroll in Federal Employees Health Benefits (FEHB) or
Change My FEHB Enrollment?..........................12
What Are the Major Events That Permit Enrollment or Change in
Can I Change My Enrollment if My Physician Stops Participating
What Happens When I Have Federal Employees Health Benefits (FEHB)
Can I Continue My Federal Employees Health Benefits (FEHB) Coverage
Can My Family Members Continue Federal Employees Health Benefits
Enrollment? ....................................13
When Does My Enrollment Become Effective? .................14
What Is an Enrollment Request? .........................14
With My Plan? ..................................15
When Will I Get an Identification Card? .....................15
Coverage and Medicare? .............................15
After I Retire? ...................................16
When Does My Enrollment Continue Automatically? ..............17
Transfer ...................................17
Leave Without Pay..............................17
Military Service ...............................17
Workers’ Compensation ...........................18
What Happens to My Family’s Coverage When I Die? .............18
Can I Cancel My Enrollment? ..........................18
When Will My Enrollment End? .........................19
Do I Get an Extension of Coverage After My Enrollment Ends? ........20
Can I Continue FEHB Coverage After I Separate From Service? ........20
How Do I Elect Temporary Continuation of Coverage? .............21
(FEHB) Coverage? ................................21
ii
How Do My Family Members Elect Temporary Continuation of Coverage? . . 21
I’m Leaving Federal Employment. Can I Get a Certificate of My
Will the Office of Personnel Management (OPM) Process or Pay
What Are My Rights and Responsibilities as a Federal Employees
What About Premiums for Temporary Continuation of Coverage? .......22
When Does My Temporary Continuation of Coverage Become Effective? . . . 22
Can I Convert to an Individual Policy? ......................23
How Do I Apply for an Individual Policy? ....................23
What Happens if I Miss the Deadline? ......................23
Can My Family Members Convert to an Individual Policy? ...........24
When Does the Individual Policy Become Effective? ..............24
FEHB Coverage? .................................24
Where Can I Get Information on How My Plan Processes Claims? .......24
My Claim? ....................................25
What Can I Do if My Plan Won’t Pay a Claim? .................25
Health Benefits (FEHB) Enrollee? ........................25
What Are the Five Steps to Safer Health Care?..................27
Table of Permissible Changes in Enrollment ...................29
Employees.....................................29
Annuitants .....................................31
Former Spouse Under Spouse Equity Provisions .................33
Temporary Continuation of Coverage Enrollees .................35
iii

What is the Federal Employees Health Benefits (FEHB) Program?
The FEHB Program is the largest employer-sponsored group health insurance program in the world,
covering almost 9 million people including employees, annuitants, and their family members, as well
as some former spouses and former employees. The FEHB Program offers fee-for-service plans, Health
Maintenance Organizations (HMOs), and plans offering a Point of Service (POS) product.
Can I Enroll?
Do I Have to Join?
You can enroll in FEHB if you are:
•
a permanent Federal employee with a regularly scheduled
tour of duty;
•
a temporary employee with an appointment for longer
than one year; or
•
a temporary employee with an appointment limited to one
year or less, and you have completed one year of current
continuous employment (excluding any break in service
of 5 days or less).
You are not eligible to enroll if you are an intermittent
employee (you don’t have a prearranged regular tour of
duty) or if your position is excluded from coverage by law
or regulation.
No, you decide whether you want to participate in the FEHB
Program. When you first become eligible, your human
resources office will ask you to choose either to enroll or not
to enroll. If you don’t enroll when you first become eligible,
you won’t be able to enroll until open season or until
another event permitting enrollment occurs.
1

What Does the Federal
Employees Health Benefits
(FEHB) Program Offer?
How Do I Stay Informed About
FEHB and Participating
Health Plans?
•
Group-rated premiums and benefits;
•
A Government contribution toward the cost of your plan;
•
Your choice of plans and options;
•
Annual enrollment opportunities (called open season);
•
Guaranteed coverage that your plan can’t cancel;
•
No waiting periods, medical examinations or restrictions
because of age or physical condition;
•
Catastrophic protection against unusually large medical
bills;
•
Salary deduction for premiums;
•
Temporary continuation of FEHB coverage or conversion
to an individual contract after your enrollment or a family
member’s coverage ends;
•
Continued group coverage into retirement or while you
are receiving Workers’ Compensation;
•
Continued group coverage for your family after you die.
Before you enroll, your human resources office will give
you a copy of the most current Guide to Federal Employees
Health Benefits Plans. Use that to decide which health plans
you are interested in, and request those plans’ brochures
from your human resources office. Read the brochures
carefully to find out what each plan covers, its rules, its
exclusions, and its limitations. Once you enroll, your health
plan will send you an updated brochure every year that
specifies how it changes for the upcoming year. If you want
to continue your current enrollment, you don’t have to do
anything during open season.
You can download Guides and plan brochures from our web
site at www.opm.gov/insure. You can also compare health
plans, link to plan web sites, and get information on plan
quality. You can access the FEHB Handbook, which
contains policies, procedures, and guidance for enrollees and
employing offices on the FEHB Program. If your agency
participates in Employee Express, you can make enrollment
changes online during open season. Our web site has the
most current information available to you.
2

Do I Pay for Federal Employees
Health Benefits (FEHB)
Coverage?
What Is Premium Conversion?
You share the cost of your health benefits coverage with the
Government. Most full-time employees pay only 25% of the
total premium.
Premiums and the Government contribution change yearly.
You can find each plan’s current premiums in the most
recent Guide to Federal Employees Health Benefits Plans
(available from your human resources office and at
www.opm.gov/insure
).
If you are a part-time employee, your share of the premiums
will be greater than for a full-time employee. Ask your
human resources office for information about the cost of
your enrollment.
If you are a temporary employee, former spouse, or person
enrolled under temporary continuation of coverage, the
Government does not contribute toward the cost of your
enrollment. You must pay both the Government and
employee shares of the cost.
Premium conversion is a method of reducing your taxable
income by the amount of your FEHB insurance premium.
Section 125 of the Internal Revenue Code allows your
employer to provide a portion of your salary in pre-tax
benefits rather than in cash. The effect is that your taxable
income is reduced. You save on:
•
Federal income tax,
•
Social Security tax,
•
Medicare tax, and
•
State and local income tax (in most States and localities).
Premium conversion has no effect on:
•
statutory pay provisions,
•
the General Schedule,
•
the amount of your health insurance premium,
•
the Government contribution towards your FEHB
premium, or
•
your base pay for retirement, life insurance, or the Thrift
Savings Plan.
3

What Is Premium Conversion?
(continued)
You are automatically enrolled in premium conversion
effective the first pay period on or after October 1, 2000, if
you are an active employee of the Executive Branch of the
Federal Government and you participate in the Federal
Employees Health Benefits (FEHB) Program. If the
Executive Branch does not employ you, or an Executive
Branch agency does not issue your pay, you may participate
in premium conversion if your employer offers it. The
Federal Judiciary, the U.S. Postal Service, and some
Executive Branch agencies with independent
compensation-setting authority already offer their own
premium conversion plans.
You may only waive participation in premium
conversion:
•
At the initial premium conversion effective date;
•
During an open season;
•
When you are first hired or hired as a reemployed
annuitant;
•
When you leave Federal service and are rehired in a
different calendar year; or
• When you have a qualifying life event (whether or not
you change your FEHB enrollment).
You can cancel your waiver and participate in premium
conversion:
•
When you have a qualifying life event; or
•
During an open season.
Retirees and persons paying FEHB premiums directly (not
by payroll deduction) are not eligible for premium
conversion.
A qualifying life event includes:
•
Addition of a dependent;
•
Birth or adoption of a child;
•
Changes in entitlement to Medicare or Medicaid for you,
your spouse, or dependent;
•
Change in work site;
4

•
Change in your employment status or that of your spouse
or dependent from either full-time to part-time, or the
reverse;
•
Death of your spouse or dependent;
•
Divorce or annulment;
•
Loss of a dependent;
•
Marriage;
•
Significant change in the health coverage of you or your
spouse related to your spouse’s employment;
•
Start or end of an unpaid leave of absence by you or your
spouse; or
•
Start or end of your spouse’s employment.
What Types of Plans Are The types of plans that participate in the Federal Employees
Health Benefits (FEHB) Program are:
Available?
Fee-for-Service Plans
This is a traditional type of insurance in which the health
plan will either reimburse you or pay the medical provider
directly for each covered medical expense after you receive
the service. When you need medical attention, you visit the
doctor or hospital of your choice. After receiving medical
treatment, your provider or you file a claim to your health
plan and it pays a benefit, but you usually must first pay a
deductible and coinsurance or a copayment. These plans use
some managed care features such as precertification and
utilization review to control costs. Most also provide access
to preferred provider organizations (PPOs), as described
below. When you use a PPO, you do not have to file a
claim. Using a PPO will save you money.
Fee-for-service plans include:
•
Plans open to everyone eligible to enroll under the FEHB
Program. Some of these plans are sponsored by unions or
employee organizations that require you to hold full or
associate membership in the sponsoring organization.
5

What Types of Plans Are
•
Plans sponsored by unions and employee organizations
and restricted to employees in certain occupational groups
and/or agencies.
Available? (continued)
Generally, a sponsoring organization will require you to pay
a membership fee or dues, in addition to the premium. The
employee organization sets and collects this fee, which is
not negotiated with the Office of Personnel Management
(OPM).
•
Preferred Provider Organizations (PPO). A PPO is a
fee-for-service option that allows you to see certain
medical providers who reduce their charges to the plan,
which means you pay less money out-of-pocket than
when you use a non-PPO provider. When you visit a PPO
you usually won’t have to file claims or paperwork.
However, going to a PPO hospital does not guarantee
PPO benefits for all services received within that hospital.
For instance, the PPO agreement may not cover lab work
and radiology services from independent practitioners
within the hospital, but it would cover room and board
charges.
Health Maintenance Organizations (HMOs)
An HMO is a health plan that provides care through a
network of physicians, hospitals, and other providers in
particular geographic areas. HMOs coordinate the health
care services you receive. Your eligibility to enroll in an
HMO is determined by where you live or, for some plans,
where you work. Some HMOs have agreements with
providers in other service areas for non-emergency care if
you travel or are away from home for extended periods,
called “reciprocity”. Plans that offer such reciprocity discuss
it in their benefit brochure under Special Features.
•
The HMO provides a comprehensive set of services – as
long as you use the doctors and providers in the HMO
network. HMOs charge a copayment for primary
physician and specialist visits and generally no deductible
or coinsurance for in-hospital care.
•
Most HMOs ask you to choose a doctor or medical group
to be your primary care physician (PCP). Your PCP
6

What Types of Plans Are
Available? (continued)
What Types of Enrollment Are
Available?
provides your general medical care. In many HMOs, you
must get authorization or a “referral” from your PCP for
you to be evaluated and/or treated by a different physician
or medical professional. The referral ensures that you see
the right provider for the care most appropriate to your
condition.
•
Care you receive from a provider not in the HMO’s
network is not covered unless it’s emergency care, you
have obtained a proper referral for the care, or the plan
has a reciprocity arrangement.
Point of Service
Some fee-for-service plans and health maintenance
organizations (HMOs) offer a point of service product. You
have the choice of using a designated network of providers
or going outside of the network for care. If you use network
providers, your out-of-pocket costs will be less than if you
go out of network. If you don’t use network providers, you
must pay higher out-of-pocket costs, including deductibles,
coinsurance, and copayments.
The Federal Employees Health Benefits (FEHB) Program
offers two types of enrollment:
Self Only
A self only enrollment covers only you as the enrollee. If
you have a self only enrollment and want to cover a new
family member, you must change to a self and family
enrollment.
Self and Family
A self and family enrollment covers you and all of your
eligible family members. You can not exclude any eligible
family member from coverage. You can not provide
coverage for anyone who is not an eligible family member,
even if they live with you and are dependent upon you.
7

What Types of Enrollment Are
Available? (continued)
Which Family Members Are
Covered Under My Enrollment?
A new family member is automatically covered under your
self and family enrollment. You do not need to report the
addition of a new family member to your human resources
office, but your plan may ask you for information (such as a
marriage license or birth certificate) to verify the family
member’s eligibility. Your plan is not entitled to a new
enrollment form as verification of the family member’s
eligibility.
The family members covered under your self and family
enrollment are:
•
Your spouse;
•
Your unmarried dependent children under age 22. In
addition to natural children of a marriage, this includes:
•
Your legally adopted child;
• Your recognized natural child, if you live together
in a parent-child relationship, or the child is
financially dependent upon you, or if there is a
judicial determination of support;
• Your stepchild, if you live together in a
parent-child relationship; and
• Your foster child, if you live together in a
parent-child relationship and you expect to raise
the child to adulthood (this may include a
grandchild);
•
Your unmarried dependent child age 22 or over who is
incapable of self-support because of a disability that
existed before age 22. You must expect the disability to
continue for at least one year, and the disability must be
the reason the child isn’t capable of self-support.
The Federal Employees Health Benefits (FEHB) Handbook
provides more detailed guidance on coverage requirements,
including certifications that you must complete to cover a
foster child or a child incapable of self-support (see
www.opm.gov/insure/handbook/FEHB28.htm
).
8

When Does My Family Member
Lose Coverage?
When Can I Change From a
Self and Family Enrollment To
a Self Only Enrollment?
Your spouse immediately loses coverage under your self
and family enrollment when your divorce decree or
annulment is final (according to State law).
Your child immediately loses coverage under your self and
family enrollment when:
•
Your child reaches age 22, unless he/she is incapable of
self support;
•
Your child marries;
•
Your disabled child age 22 or over marries or becomes
capable of self-support; or
•
Your stepchild or foster child stops living with you in a
parent-child relationship.
Your family member will get a 31-day extension of
coverage. He/she will be eligible to elect temporary
continuation of Federal Employees Health Benefits (FEHB)
coverage or may elect to convert coverage to an individual
contract. Your former spouse may be eligible to enroll for
FEHB coverage under Spouse Equity provisions.
Your family members also lose coverage if you change from
a self and family to a self only enrollment.
Neither your human resources office nor your plan will
notify you when your family member loses eligibility.
You should immediately tell your plan when a family
member loses coverage. If your plan pays for services
received after your family member’s coverage ends, you
must repay the plan.
If you participate in premium conversion, you may change
to a self only enrollment during the annual open season or
within 60 days after you have a qualifying life event. The
change in enrollment must be consistent with your
qualifying life event. For example, if you get divorced,
changing to a self only enrollment would be consistent with
that qualifying life event. If you adopt a child, a change
from self and family to self only coverage would not be
consistent with that qualifying life event.
9

When Can I Change From a
Self and Family Enrollment To
a Self Only Enrollment?
(continued)
Can My Former Spouse
Continue Federal Employees
Health Benefits (FEHB)
Coverage?
If you have waived participation in premium conversion,
you may change to a self only enrollment or cancel your
enrollment at any time.
Your former spouse may be eligible to continue FEHB
coverage under Spouse Equity if your former spouse:
•
was divorced from you during your Federal employment
or receipt of annuity;
•
was covered as a family member under an enrollment at
least one day during the 18 months before your marriage
ended;
•
is entitled to a portion of your annuity or to a former
spouse survivor annuity; and
•
does not remarry before age 55.
You or your former spouse must apply to your human
resources office for Spouse Equity coverage within 60 days
from the divorce. For more information on how your former
spouse can enroll, ask your human resources office for
Benefits for Former Spouses under the Federal Employees
Health Benefits Program or see the FEHB Handbook at
www.opm.gov/insure/handbook/FEHB31.htm
.
If your former spouse is not eligible to enroll under Spouse
Equity, he/she may be eligible to continue FEHB coverage
under Temporary Continuation of Coverage provisions.
10

Can Someone Be Covered
Under More Than One Federal
Employees Health Benefits
(FEHB) Enrollment?
Generally, you may not be covered under two plans at the
same time. A human resources office may authorize a dual
enrollment to:
•
Protect children who would otherwise lose coverage as
family members; or
•
Allow an employee under age 22 covered under a parent’s
self and family enrollment to cover his/her dependent
child.
No enrollee or family member may receive benefits under
more than one FEHB enrollment. When your human
resources office authorizes a dual enrollment, you must
notify the plan(s) which family members are to be covered
under each enrollment.
For more information on dual enrollments, contact your
human resources office or see the FEHB Handbook at
www.opm.gov/insure/handbook/FEHB10.htm
.
11

When Can I Enroll in Federal
Employees Health Benefits
(FEHB) or Change My FEHB
Enrollment?
I am … When Can I Enroll?
A new employee. Within 60 days after your
appointment date.
Moving to a position that
Within 60 days after your
offers FEHB coverage. My
appointment date.
previous position was excluded
from coverage.
An eligible employee, but I am Open season, or when another
not enrolled in FEHB. event permitting enrollment
occurs (such as a change in
family status or employment
status).
Enrolled in FEHB, and I want Open season, or when another
to change my enrollment. event permitting enrollment
occurs (such as a change in
family status or employment
status).
If you are an eligible temporary employee, all of the
enrollment and enrollment change information applies to
you with one exception. A decision not to enroll will not
affect your future eligibility to continue FEHB enrollment
after retirement.
To enroll or change your enrollment, you must file an
enrollment request with your human resources office within
the time limit shown in the Table of Permissible Changes in
Enrollment (see pages 29-36).
Important: You will not be eligible for FEHB coverage
after retirement unless you are enrolled before you retire and
meet all the requirements for continuing enrollment after
retirement (see page 16).
12

What Are the Major Events
That Permit Enrollment or
Change in Enrollment?
•
A change in family status:
3
marriage
3
birth or adoption of a child
3
acquisition of a foster child
3
legal separation
3
divorce
•
A change in employment status:
3
you are reemployed after a break in service of more
than 3 days
3
you return to pay status after your coverage terminated
during leave without pay status or because you were in
leave without pay status for more than 365 days
3
your pay increases enough for premiums to be withheld
3
you are restored to a civilian position after serving in
the uniformed services
3
you change from a temporary appointment to an
appointment that entitles you to a Government
contribution
3
you change to or from part-time career employment.
• You or a family member lose Federal Employees Health
Benefits (FEHB) or other coverage:
3
under another FEHB enrollment because the covering
enrollment was terminated, canceled, or changed to self
only
3
under another federally-sponsored health benefits
program
3
under Medicaid or similar State-sponsored program for
the needy
3
because your membership terminates in the employee
organization sponsoring the FEHB plan
3
under a non-Federal health plan.
•
When one of these events occur, you may:
3
enroll
3
change your enrollment from self only to self and
family
3
change your enrollment to another FEHB plan or
option.
13

What Are the Major Events
That Permit Enrollment or
Change in Enrollment?
(continued)
When Does My Enrollment
Become Effective?
What Is an Enrollment Request?
You also may waive or cancel your waiver of premium
conversion at the same time (see “What Is Premium
Conversion?”).
You must give your enrollment change to your human
resources office from 31 days before to 60 days after the
event.
See the Table of Permissible Changes in Enrollment for
other enrollment and enrollment change opportunities.
Generally, the effective date of your enrollment or
enrollment change is the first day of the pay period that
follows:
•
the day your human resources office receives your
completed enrollment request; and
•
a pay period during any part of which you were in pay
status. (This pay status requirement doesn’t apply to a
change from self only to self and family.)
However, some events, such as open season, have different
effective dates. You can find complete information about
effective dates in the Federal Employees Health Benefits
(FEHB) Handbook at
www.opm.gov/insure/handbook/FEHB10htm
.
You may use the Health Benefits Election form (SF 2809) to
request a new enrollment or change in enrollment. The
SF 2809 may be in either paper or electronic format. In
addition, your human resources office may also allow you to
make open season changes through “Employee Express” or
another electronic method, which doesn’t involve a
SF 2809.
14

Can I Change My Enrollment
if My Physician Stops
Participating With My Plan?
When Will I Get an
Identification Card?
What Happens When I Have
Federal Employees Health
Benefits (FEHB) Coverage and
Medicare?
No, this is not a qualifying event for changing your
enrollment. However, if you have a chronic or disabling
condition and your health plan terminates your provider’s
contract (unless the termination is for cause), you may be
able to continue seeing your provider for up to 90 days after
the notice of termination. If you are in the second or third
trimester of pregnancy, you may continue seeing your
obstetrician until the end of postpartum care.
Your plan will send you an identification card once it
processes your enrollment. If you need services before you
get your identification card, use your copy of the Health
Benefits Election form (SF 2809) or your Employee Express
enrollment verification letter as proof of enrollment.
Generally, your FEHB plan and Medicare provide protec-
tion against the same kind of medical expenses. Your FEHB
plan also provides prescription drug coverage, routine
physicals and a wider range of preventive services that
Medicare does not. Some FEHB plans also provide coverage
for dental and vision care. Medicare covers orthopedic and
prosthetic devices, durable medical equipment, home health
care, limited chiropractic services, and medical supplies,
which some FEHB plans may not cover or only partially
cover (check your plan brochure for details).
Whether your FEHB plan or Medicare is primary depends
on your current employment or health status. Your FEHB
plan brochure provides specific information on how its
benefits are coordinated with Medicare.
You can get more information about Medicare at
www.medicare.gov or from the publication
Medicare and
You (also available on the web site). You can get more
information on FEHB plans and Medicare in the booklet
entitled “The Federal Employees Health Benefits Program
and Medicare,” at
www.opm.gov/insure/MCare/MHB01.htm
.
15

Can I Continue My Federal
Employees Health Benefits
(FEHB) Coverage After I
Retire?
You may continue your FEHB enrollment after you retire if:
•
you are entitled to retire on an immediate annuity under a
retirement system for Federal civilian employees; and
•
you have been continuously enrolled (or covered as a
family member) in any FEHB plan(s) for the 5 years of
service immediately before your annuity starts, or for the
full period of service since your first opportunity to enroll
(if less than 5 years).
An immediate annuity is one that begins within 30 days of
separation for retirement. An annuity you receive under the
Minimum Retirement Age (MRA)+10 provision of the
Federal Employees Retirement System (FERS) also
qualifies as an immediate annuity, even though you
postponed receipt of your annuity after separating from
service.
“Service” means time in a position in which you were eligi-
ble to be enrolled and receive a Government contribution
towards the cost of your enrollment. You do not need to
have been enrolled in the same FEHB plan. Coverage under
a non-FEHB plan doesn’t count toward the five-year or
first-opportunity requirement, except that time covered
under TRICARE counts as long as you are covered under an
FEHB enrollment when you retire.
Your first opportunity to enroll is within 60 days after you
first become eligible to enroll and receive a Government
contribution towards the cost of your enrollment.
The Office of Personnel Management (OPM) may waive the
five-year requirement for continuation of enrollment after
retirement only under exceptional circumstances. For more
information on OPM’s waiver authority, see the FEHB
Handbook at www.opm.gov/insure/handbook/FEHB22.htm.
16

When Does My Enrollment
Continue Automatically?
Transfer
Your Federal Employees Health Benefits (FEHB)
enrollment will continue when you transfer from one agency
to another, as long as you:
•
don’t have a break in service of more than three calendar
days; and
•
are eligible for FEHB coverage in your new position.
Leave Without Pay
Your FEHB enrollment will continue for up to one year
while you are in leave without pay status, unless you cancel
it. You must pay your share of the premiums. Your human
resources office will tell you how to make the premium
payments.
Military Service
Your FEHB enrollment will continue without change if you
enter on active duty in the military service for 30 days or
less.
If you enter on active duty for more than 30 days, you may
continue your FEHB enrollment for up to 18 months. You
may have to pay your share of the premiums for the first 12
months, and you may have to pay an additional amount to
continue coverage during the last 6 months of the 18-month
period. Your human resources office will tell you whether
you will have to pay premiums, how much the premiums
will be, and how to make the premium payments.
You may also choose to terminate your enrollment. You will
get it back when you exercise your reemployment rights and
return to civilian service. Your decision to terminate your
enrollment will not affect your future eligibility to continue
FEHB enrollment after retirement as long as you enroll
within 60 days after you return to civilian service.
17

When Does My Enrollment
Continue Automatically?
(continued)
What Happens to My Family’s
Coverage When I Die?
Can I Cancel My Enrollment?
Workers’ Compensation
Your enrollment continues while you are receiving
compensation from the Office of Workers’ Compensation
Programs (OWCP) if:
•
OWCP determines that you are unable to return to duty;
and
•
you meet the same requirements for continuing coverage
as for retirement.
Your surviving eligible family members may continue your
health benefits enrollment after you die if:
•
you had a self and family enrollment; and
•
one family member is entitled to a survivor annuity.
Your retirement system will take appropriate action with
your survivors.
If you participate in premium conversion, you may cancel
your enrollment only during an open season or upon a
qualifying life event. The cancellation of coverage must be
consistent with and correspond to your qualifying life event.
For example, if you get married and your spouse is
employed by a company that provides health insurance for
you, then canceling Federal Employees Health Benefits
(FEHB) coverage would be consistent with that qualifying
life event. If you are divorcing and have children to cover,
canceling coverage would not be consistent with that
qualifying life event.
If you have waived participation in premium conversion,
you may cancel your enrollment at any time.
Your cancellation takes effect on the last day of the pay
period in which your human resources office receives your
request. You and your family members are not eligible for
the 31-day extension of coverage, Temporary Continuation
of Coverage, or conversion to an individual policy.
18

Can I Cancel My Enrollment?
(continued)
When Will My Enrollment End?
When you cancel your enrollment, you may not enroll again
until an event occurs (such as an open season or a change in
family status) that permits enrollment.
You will not be eligible for health benefits coverage after
your retirement unless you reenroll before you retire and
meet all of the requirements for continuing enrollment into
retirement. If you plan to reenroll in time to qualify for
coverage as a retiree, keep in mind that you may have to
retire earlier than expected. You then might not meet the
five-year requirement for continuing coverage into retire-
ment. When you cancel your enrollment you are
accepting this risk. You may want to consider changing
your enrollment to a lower cost plan instead of cancellation.
If you are going to be covered by someone else’s enrollment
and do not want a gap in coverage, you can coordinate the
effective dates of your cancellation and your new coverage.
Your enrollment will end, subject to a 31-day extension of
coverage, when you:
•
separate from service (unless you can retire and continue
your enrollment);
•
separate under the Federal Employees Retirement System
(FERS) MRA+10 provision and you postpone receiving
your annuity (you will get Federal Employees Health
Benefits [FEHB] coverage back when your annuity
starts);
•
change to a position that is excluded from coverage;
•
die (your family may be eligible to continue coverage);
•
have been on leave without pay for 365 consecutive days,
or when your leave under the Family and Medical Leave
Act expires, whichever is later;
•
return to leave without pay status, if you haven’t been in
pay status for 4 consecutive months after 365 days of
continued coverage while in leave without pay status;
•
enter on active duty in the military service for more than
30 days, if you decide to terminate your enrollment;
•
have completed 18 months of active duty in the military
service, or your entitlement to continued coverage ends,
whichever is earlier; or
19

When Will My Enrollment
End? (continued)
Do I Get an Extension of
Coverage After My Enrollment
Ends?
Can I Continue FEHB Coverage
After I Separate From Service?
•
are a temporary employee whose pay is not enough to
cover the premiums and you do not choose a lower-cost
plan.
See the Federal Employees Health Benefits (FEHB)
Handbook at www.opm.gov/insure/handbook/FEHB15.htm
for the effective dates of termination actions.
Your coverage will continue without cost to you for 31 days
after your enrollment ends for any reason except when you
cancel it. During that time you can elect Temporary
Continuation of Coverage (TCC) or convert to an individual
health benefits contract with your FEHB plan. Important:
you must exhaust TCC eligibility as one condition for
guaranteed access to individual health coverage under the
Health Insurance Portability and Accountability Act of
1996.
Your family members are eligible for the extension of
coverage when they lose coverage for any reason except
when you cancel your enrollment.
If you are hospitalized on the 31
st
day of extended coverage,
your FEHB plan will continue to provide benefits for up to
60 more days of continuous hospitalization unless you
converted to an individual contract.
You are eligible to temporarily continue your FEHB
coverage for up to 18 months when you:
•
separate from service, voluntarily or involuntarily, unless
your separation is for gross misconduct; and
•
are not otherwise eligible for continued coverage under
the Program (not counting the 31-day extension of
coverage).
You can get more details on Temporary Continuation of
Coverage (TCC) from the FEHB Handbook at
www.opm.gov/insure/handbook/FEHB15.htm
or from the
booklet Temporary Continuation of Coverage under the
Federal Employees Health Benefits Program (RI 79-27).
20

How Do I Elect Temporary
Continuation of Coverage?
Can My Family Members
Continue Federal Employees
Health Benefits (FEHB)
Coverage?
How Do My Family Members
Elect Temporary Continuation
of Coverage?
Your human resources office will give you notice of your
Temporary Continuation of Coverage (TCC) rights within
61 days after you separate from service. If you want TCC,
you must elect it within 60 days from the later of:
•
your separation; or
•
the date of your human resources office’s notice.
You may choose self only or self and family coverage in any
plan or option that you are eligible to join. You are not
limited to the plan, option, or type of enrollment under
which you had been covered.
Your family members are eligible to continue FEHB
coverage for up to 36 months under their own Temporary
Continuation of Coverage (TCC) enrollments when they:
•
lose their eligibility under your coverage; and
•
are not otherwise eligible for FEHB coverage.
This includes when your child reaches age 22 or marries, or
when you divorce and your former spouse does not qualify
under Spouse Equity provisions. Neither your human
resources office nor your plan will notify you or your
family member when he/she loses coverage.
Your family members are not eligible for TCC when you
cancel your enrollment or change to a self only enrollment.
You must notify your human resources office or retirement
system within 60 days from the date that your family
member loses eligibility under your enrollment. (If you are
divorcing, your former spouse may notify your human
resources office on his/her own behalf.) Within 14 days,
your human resources office will send your family member
notice of his/her own Temporary Continuation of Coverage
(TCC) rights.
If your family member wants TCC, he/she must elect it
within 60 days from the later of:
21

How Do Family Members Elect
Temporary Continuation of
Coverage? (continued)
What About Premiums for
Temporary Continuation of
Coverage?
When Does My Temporary
Continuation of Coverage
Become Effective?
•
the date he/she loses eligibility under your enrollment; or
•
the date of your human resources office’s notice.
If your former spouse loses Spouse Equity eligibility within
36 months after your marriage ends, he/she must notify your
human resources office within 60 days of losing this
eligibility to apply for the remaining months of TCC.
Generally, you or your family member must pay both the
Government and employee shares of the premium, plus a
2% administrative charge. When Temporary Continuation of
Coverage (TCC) ends, you will get another 31-day
extension of coverage and conversion rights (unless you
canceled your coverage or did not pay premiums).
The first 31 days of the Temporary Continuation of
Coverage (TCC) eligibility period overlap with the free
31-day extension of coverage. You must begin to pay
premiums for TCC after the 31-day extension of coverage
ends. You must pay retroactive premiums to this date even if
your enrollment is not finalized by then.
If you:
•
elect a different plan or option when you enroll under
TCC, and
31
•
you or a covered family member are in a hospital on the
st
day of the extension of coverage,
your old plan or option will continue coverage for the
hospitalized person as long as he/she is hospitalized, up to
60 days. The other family members’ coverage will switch to
the new plan or option after the 31-day extension of
coverage ends.
22

Can I Convert to an Individual
Policy?
How Do I Apply for an
Individual Policy?
What Happens if I Miss the
Deadline?
You may convert to an individual policy with the carrier of
your plan when your Federal Employees Health Benefits
(FEHB) coverage ends, except when you cancel your
enrollment.
The plan is not allowed to:
•
ask for evidence of good health;
•
impose waiting periods; or
•
limit coverage for pre-existing conditions.
Your benefits and rates will be different from those under
the FEHB Program. The Government does not contribute to
the cost of the individual conversion contract.
Your human resources office must give you a notice of your
right to convert to an individual policy no later than 60 days
from the termination date.
Complete the back of your copy of the notice and send it to
the carrier of your plan within 31 days from the date of the
notice, but no later than 91 days from the date your
enrollment terminates.
You lose your opportunity to convert to an individual policy
unless there are reasons beyond your control (including
when you do not get the required conversion notice within
60 days). In those cases, you can ask the carrier of your plan
to accept a late conversion. You must send your written
request within 6 months after the date your enrollment
terminated. You must include some documentation that your
enrollment has terminated (for example, a Notification of
Personnel Action, SF 50 showing separation from service).
23

Can My Family Members
Convert to an Individual Policy?
When Does the Individual Policy
Become Effective?
I’m Leaving Federal
Employment. Can I Get a
Certificate of My FEHB
Coverage?
Where Can I Get Information
on How My Plan Processes
Claims?
Your family members also may convert to individual
coverage when they lose eligibility under your enrollment,
or when their Spouse Equity or Temporary Continuation of
Coverage (TCC) ends. Neither your human resources
office nor your plan will notify you or your family member
when he/she loses coverage.
You or your family member should write to the carrier of
your plan within 31 days after your family member’s
Federal Employees Health Benefits (FEHB) coverage ends
to request conversion to an individual contract.
Your or your family member’s conversion contract becomes
effective at the end of the 31-day extension of coverage,
even when you or your family member are hospitalized on
the 31
st
day of extended coverage.
When your FEHB coverage ends, your plan will automati-
cally send you a Certificate of Group Health Plan Coverage.
You need to show this certificate to a new non-FEHB
insurer to reduce or eliminate any pre-existing condition
limitations that it may otherwise be able to apply to your
coverage. If you do not get a certificate automatically, the
plan must send you one at your request. If needed, you also
may get certificates from other FEHB plans you have been
enrolled in to document continued group health plan cover-
age.
You can get this information by reading your plan brochure
carefully. It will help you become familiar with your plan’s
benefits and claims procedures. You may also ask your plan
directly about benefits, claims payment and claims
processing.
24

Will the Office of Personnel
Management (OPM) Process or
Pay My Claim?
What Can I Do if My Plan
Won’t Pay a Claim?
What Are My Rights and
Responsibilities as a Federal
Employees Health Benefits
(FEHB) Enrollee?
No, OPM does not pay or process claims.
Your plan brochure has detailed information on how to file a
reconsideration request with your plan and a disputed claim
request with OPM. Before you request reconsideration from
the plan or ask OPM for a disputed claim review, please
read this information in your plan brochure.
A mainstay of the FEHB Program is the Patients’ Bill of
Rights and Responsibilities, as recommended by the
President’s Advisory Commission of Consumer Protection
and Quality in the Health Care Industry. The following are
consumer protections and quality initiatives you can count
on from your FEHB plan.
•
Transitional care:
3
If you have a chronic or disabling condition and your
health plan terminates your provider’s contract (unless
the termination is for cause), you may be able to
continue seeing your current specialist for up to 90
days after the notice of termination. If you are in the
second or third trimester of pregnancy, you may
continue seeing your obstetrician until the end of your
postpartum care.
3
If you have a chronic or disabling condition or are in
your second or third trimester of pregnancy and your
health plan drops out of the FEHB Program, you may
be able to continue seeing your provider if you enroll in
a new FEHB plan. You may continue to see your
current specialist after your old enrollment ends, even
if he or she is not associated with your new plan, for up
to 90 days after you receive the termination notice or
through the end of postpartum care, and pay no more
than if your old enrollment had not ended.
•
You have the right to review and obtain copies of your
medical records on request. You may ask that a physician
amend a record that is not accurate, relevant, or complete.
If the physician does not amend your record, you may add
a brief statement to the record.
25
What Are My Rights and
Responsibilities as a Federal
Employees Health Benefits
(FEHB) Enrollee? (continued)
•
Direct access to women’s health care providers for routine
and preventive health care services.
•
Coverage of emergency department services for screening
and stabilization without authorization if you have reason
to believe serious injury or disability would otherwise
result.
•
Direct access to a qualified specialist within your network
of providers if you have complex or serious medical con-
ditions that need frequent specialty care. Authorizations,
when required by the plan, will be for an adequate number
of direct access visits under an approved treatment plan.
•
Assurance that there will be no “gag rules” in provider
contracts that could limit communication about medically
necessary treatment.
•
Extensive information about plan characteristics and
performance, provider network characteristics, physician
and health care facility characteristics, and care
management.
Check our web site at
www.opm.gov/insure/health/billrights.htm f
or listings of the
specific types of information that your health plan must
make available to you. You may also contact your health
plan directly for this information.
The health care system works best when you take the time to
become informed. As a responsible consumer, you should:
•
Read and understand your health benefits coverage,
limitations, and exclusions, health plan processes, and
procedures to follow when seeking care.
•
Work with your physician in developing and carrying out
a treatment plan.
•
Practice healthy habits.
26

What Are the Five Steps to Safer
Health Care?
Medical error and patient safety aren’t well understood by
most Americans. When we need vital or risky health care
services, we want to believe that someone else has made
sure that we’ll get safe care. Sadly, every hour, 10 Amer-
icans die in a hospital due to avoidable errors; another 50 are
disabled. Too many patients get the wrong medicines, the
wrong tests and the wrong diagnosis. By asking questions,
learning more and understanding your risks, you can
improve the safety of your own health care, and that of your
family members. Take these simple steps:
1. Speak up if you have questions or concerns. Choose a
doctor who you feel comfortable talking to about your
health and treatment. Take a relative or friend with you if
this will help you ask questions and understand the answers.
It’s okay to ask questions and to expect answers you can
understand.
2. Keep a list of all the medicines you take. Tell your
doctor and pharmacist about the medicines you take,
including over-the-counter medicines such as aspirin and
ibuprofen, and dietary supplements such as vitamins and
herbals. Tell them about any drug allergies you have. Ask
the pharmacist about side effects and what foods or other
things to avoid while taking the medicine. When you get
your medicine, read the label, including warnings. Make
sure it is what your doctor ordered and you know how to use
it. If the medicine looks different than you expected, ask the
pharmacist about it.
3. Make sure you get the results of any test or procedure.
Ask your doctor or nurse when and how you will get the
results of tests or procedures. If you do not get them when
expected — in person, on the phone, or in the mail — don’t
assume the results are fine. Call your doctor and ask for
them. Ask what the results mean for your care.
4. Talk with your doctor and health care team about
your options if you need hospital care. If you have more
than one hospital to choose from, ask your doctor which one
has the best care and results for your condition. Hospitals do
a good job of treating a wide range of problems. However,
for some procedures (such as heart bypass surgery), research
shows results often are better at hospitals doing a lot of these
procedures. Also, before you leave the hospital, be sure to
27

What Are the Five Steps to
Safer Health Care? (continued)
ask about follow-up care, and be sure you understand the
instructions.
5. Make sure you understand what will happen if you
need surgery. Ask your doctor and surgeon: Who will take
charge of my care while I’m in the hospital? Exactly what
will you be doing? How long will it take? What will happen
after the surgery? How can I expect to feel during recovery?
Tell the surgeon, anesthesiologist, and nurses if you have
allergies or have ever had a bad reaction to anesthesia.
Make sure you, your doctor, and your surgeon all agree on
exactly what will be done during the operation.
28

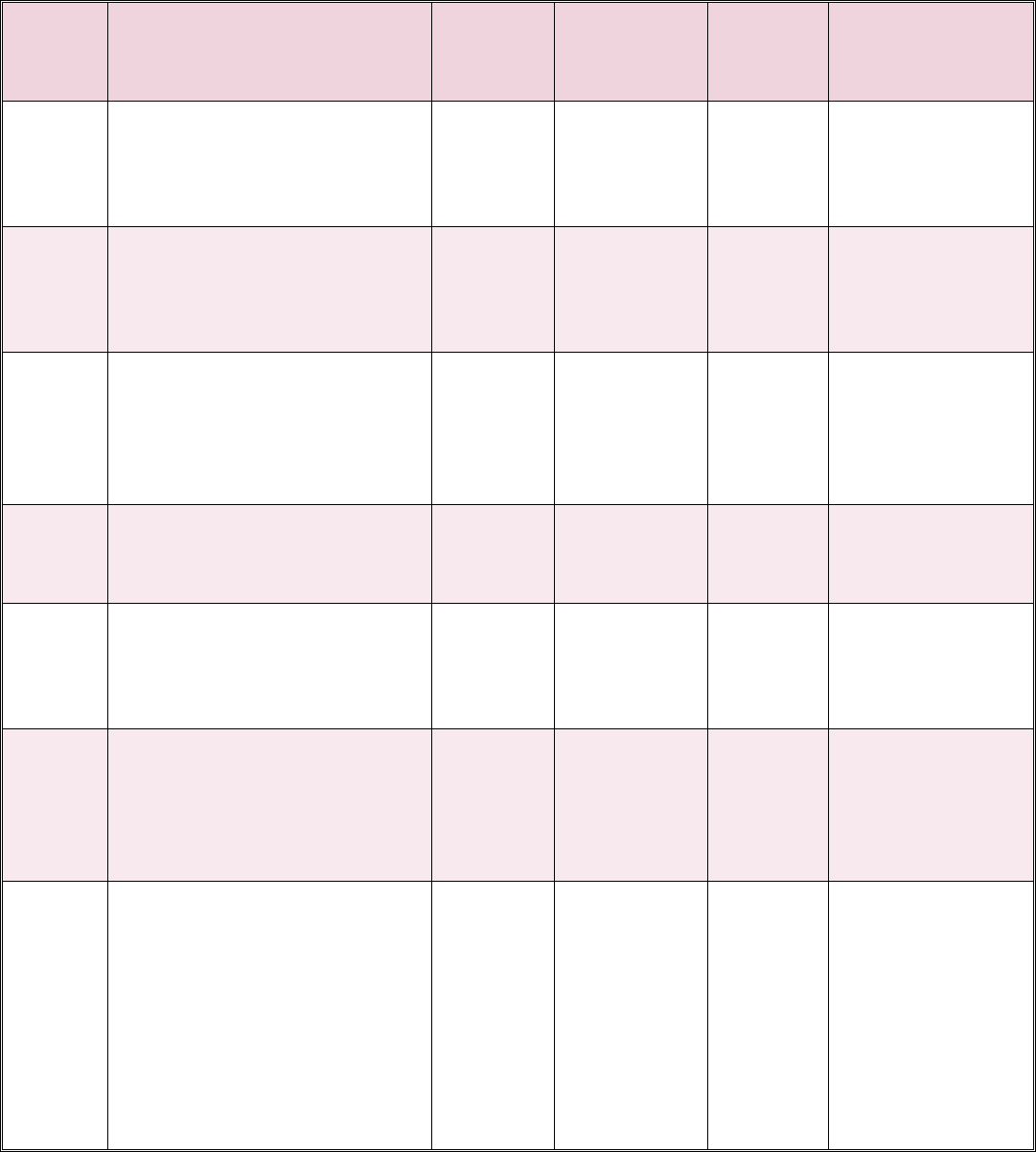
Table of Permissible Changes in Enrollment
Employees
Event
Code for
SF 2809
Events that Permit
Enrollment Changes
May
Enroll
Self Only to
Self and
Family
Change
Plans or
Options
Time Limits
1A Initial opportunity to enroll Yes N/A N/A Within 60 days
after becoming
eligible
1B Open Season Yes Yes Yes As announced by
OPM
1C Change in family status Yes Yes Yes From 31 days
before through 60
days after event
1D Change in employment status Yes Yes Yes Within 60 days of
employment status
change
1E Separation from Federal
employment when you or your
spouse are pregnant
Yes Yes Yes During final pay
period of
employment
1F Transfer from a post of duty
within United States to one
outside United States, or
reverse
Yes Yes Yes From 31 days
before leaving old
post through 60
days after arriving
at new post
1G You or eligible family member
lose coverage under FEHB or
another group insurance plan
Yes Yes Yes From 31 days
before through 60
days after date of
loss of coverage
1H You or eligible family member
lose coverage because FEHB
plan is discontinued, in whole
or part
N/A Yes Yes During open
season, unless
OPM sets a
different time
29
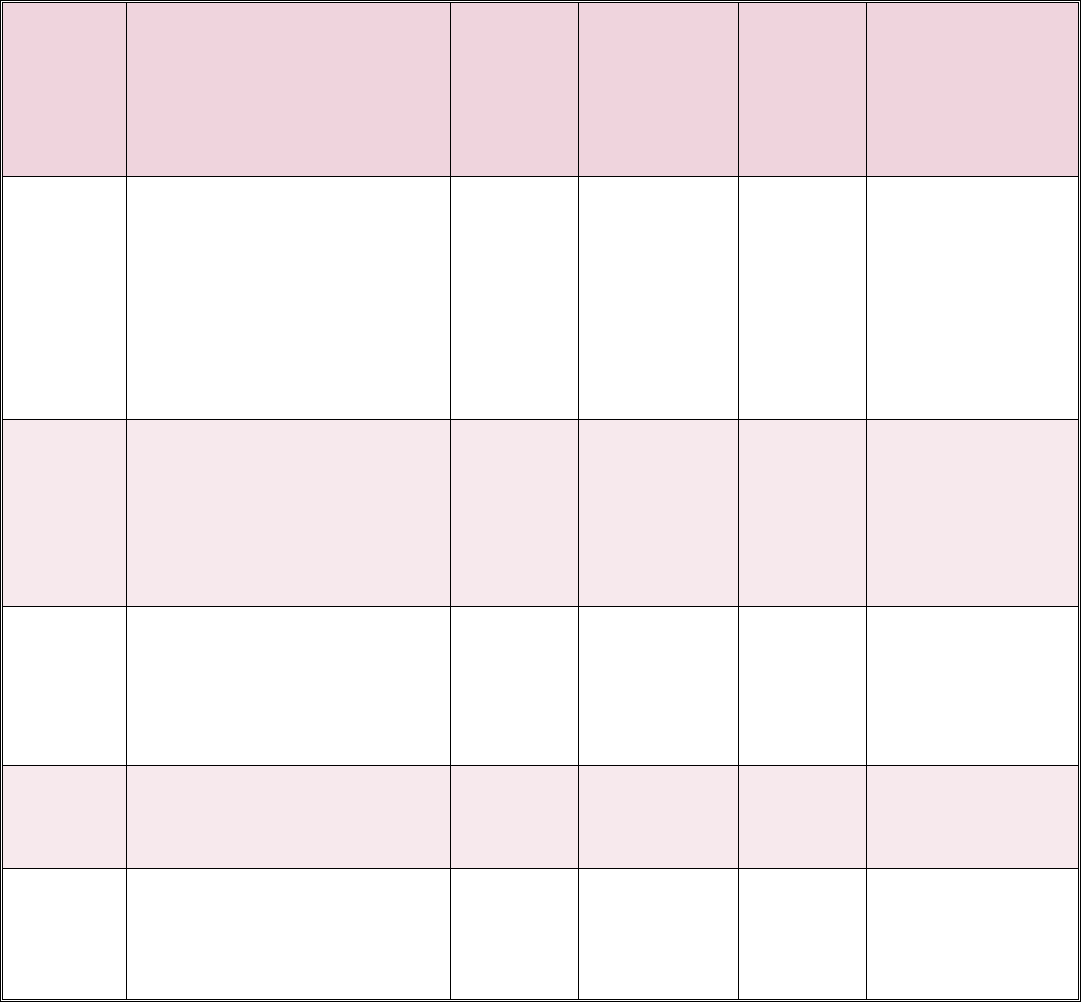
Event
Code for
SF 2809
Events that Permit
Enrollment Changes
May
Enroll
Self Only to
Self and
Family
Change
Plans or
Options
Time Limits
1I You or eligible family member
lose coverage under a
non-FEHB group health plan
because you move out of the
commuting area to accept
another position and your
non-federally employed spouse
leaves job to join you
Yes Yes Yes From 31 days
before you leave
commuting area
through 180 days
after arriving in
new commuting
area
1J You or covered family member
in an HMO move or take job
outside the service area, or if
already outside this area, move
or take job further from this
area
N/A Yes Yes Upon notifying the
human resources
office of the move
or change of place
of employment
1K On becoming eligible for
Medicare (You may make this
change only once in a
lifetime.)
N/A No Yes At any time
beginning on the
30th day before
becoming eligible
for Medicare
1L You complete one year of
continuous service as a
temporary employee
Yes N/A N/A Within 60 days
after becoming
eligible
1M Your salary as a temporary
employee is not enough to pay
for plan in which enrolled
N/A No Yes Within 60 days
after receiving
notice from human
resources office
30
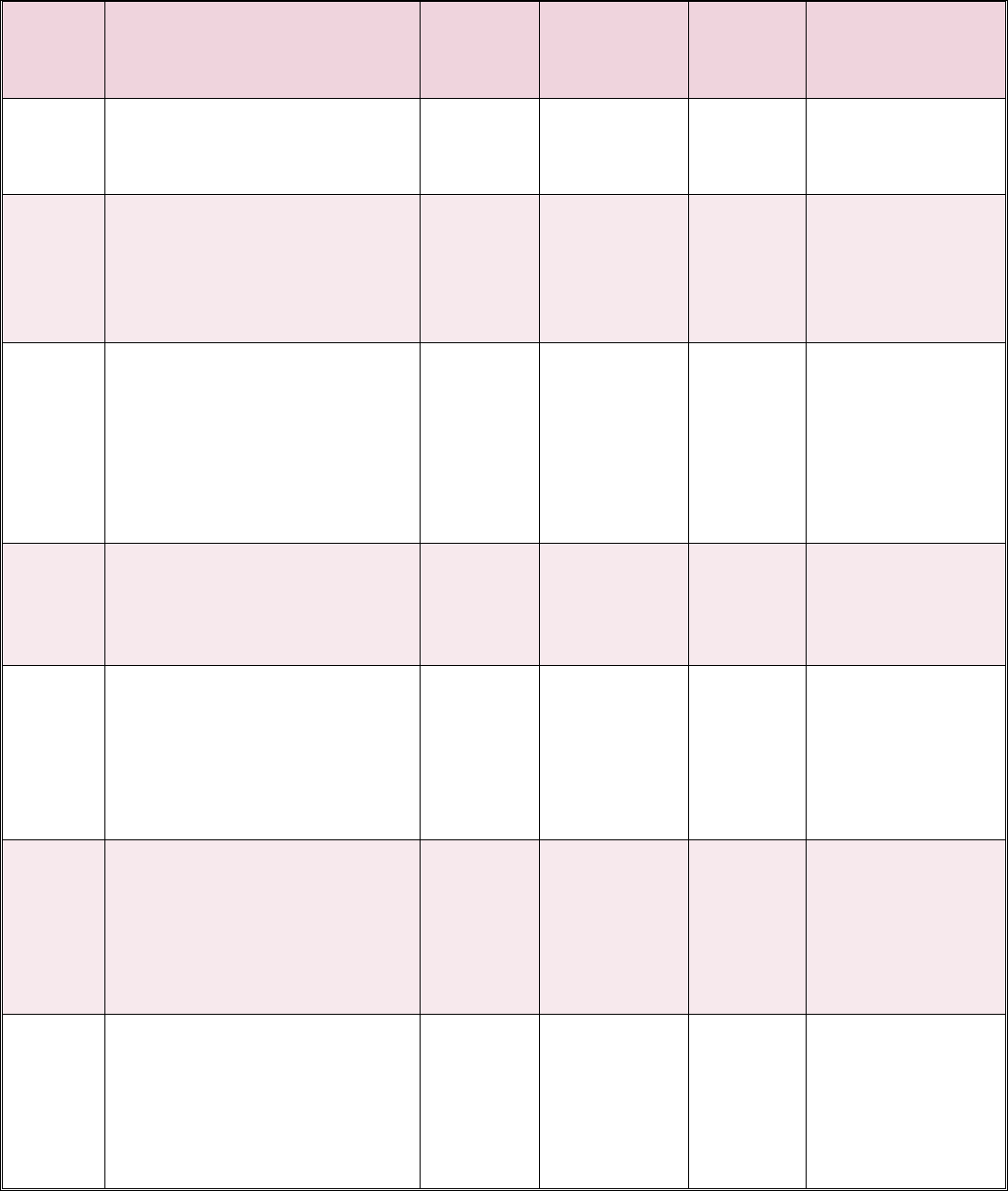
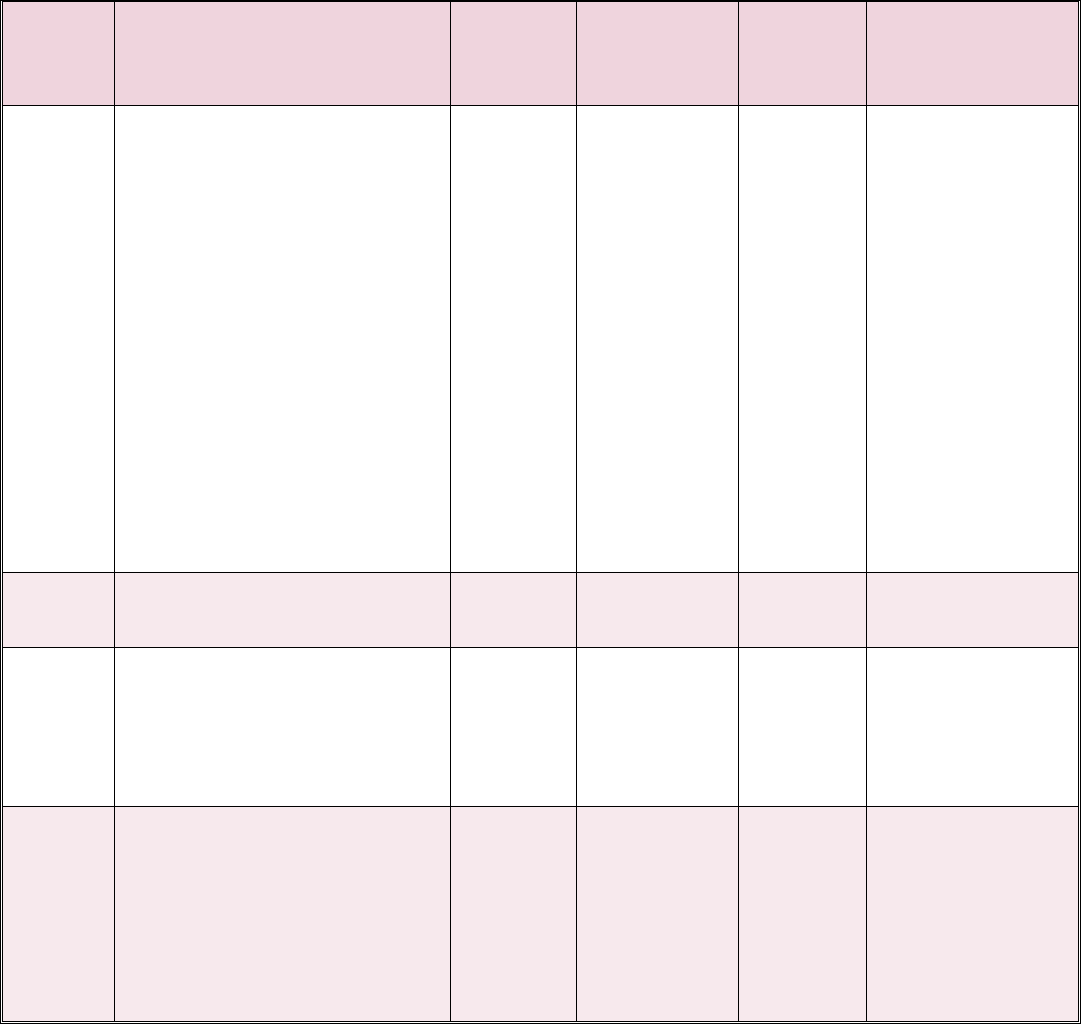
Annuitants
Event
Events that permit May Self Only to
Change
Time Limits
Code for
enrollment changes Enroll Self and
Plans or
SF 2809
Family
Options
2A Open season No Yes Yes As announced by
OPM
2B Change in family status (Special
No Yes Yes From 31 days
rules apply for survivor
annuitants; refer to the FEHB
before through 60
days after the event
Handbook)
2C Reenrollment when you
suspended FEHB enrollment to
enroll in a Medicare HMO or
Medicaid and later were
May
Reenroll
N/A N/A From 31 days
before through 60
days after
disenrollment
involuntarily disenrolled from
Medicare HMO or Medicaid
2D Reenrollment when you
May N/A N/A During open season
voluntarily disenroll from a
Reenroll
Medicare HMO or Medicaid
2E You apply for postponed
Yes N/A N/A Within 60 days
Minimum Retirement Age
(MRA)+10 annuity under the
after OPM mails
you a notice of
Federal Employees Retirement
eligibility
System (FERS)
2F Your annuity or OWCP
payments are restored
Yes N/A N/A Within 60 days
after OPM or
OWCP mails a
notice of insurance
eligibility
2G You or eligible family member
Yes Yes Yes From 31 days
lose FEHB coverage because the
through 60 days
covering enrollment was
terminated, canceled, or changed
after date of loss of
coverage
to self only
31
Event
Code for
SF 2809
Events that permit
enrollment changes
May
Enroll
Self Only to
Self and
Family
Change
Plans or
Options
Time Limits
2H You or eligible family member
lose coverage under FEHB or
another group insurance plan
No Yes Yes From 31 days
before through 60
days after loss of
coverage
2I You or eligible family member
lose coverage because FEHB
plan is discontinued in whole or
part
N/A Yes Yes During open
season, unless
OPM sets a
different time
2J You or covered family member
move or take job outside the
HMO service area, or if already
outside this area, move or take
job further from this area
N/A Yes Yes Upon notifying the
Retirement System
of the move or
change of place of
employment
2K You are in an overseas post of
duty and retire or die
No Yes Yes Within 60 days
after retirement or
death
2L You are enrolled and separate
from duty after serving 31 days
or more in a uniformed service
N/A Yes Yes Within 60 days
after separation
from the uniformed
service
2M On becoming eligible for
Medicare (You may make this
change only once in a lifetime.)
N/A No Yes At any time
beginning on the
30th day before
becoming eligible
for Medicare
2N Your annuity is not enough to
make withholdings for plan in
which enrolled
N/A No Yes Retirement system
will advise you of
the options
32
Former Spouse Under Spouse Equity Provisions
Event
Events that Permit May Self Only to
Change
Time Limits
Code for
Enrollment Changes Enroll Self and
Plans or
SF 2809
Family
Options
3A Initial opportunity to enroll Yes N/A N/A Generally, must
apply within 60
days after marriage
ends. If retiring
employee elects a
former spouse or
insurable interest
annuity, the former
spouse must apply
within 60 days after
OPM’s notice of
FEHB eligibility.
May enroll any
time after
eligibility
established
3B Open season No Yes Yes As announced by
OPM
3C Change in family status based
No Yes Yes From 31 days
on addition of family members
who are also eligible family
before through 60
days after change
members of the employee or
in family status
annuitant
3D Reenrollment of former spouse
who cancelled FEHB enrollment
to enroll in a
Medicare-sponsored HMO or
Medicaid and who later was
May
Reenroll
N/A N/A From 31 days
before through 60
days after
disenrollment
involuntarily disenrolled from
Medicare HMO or Medicaid
33
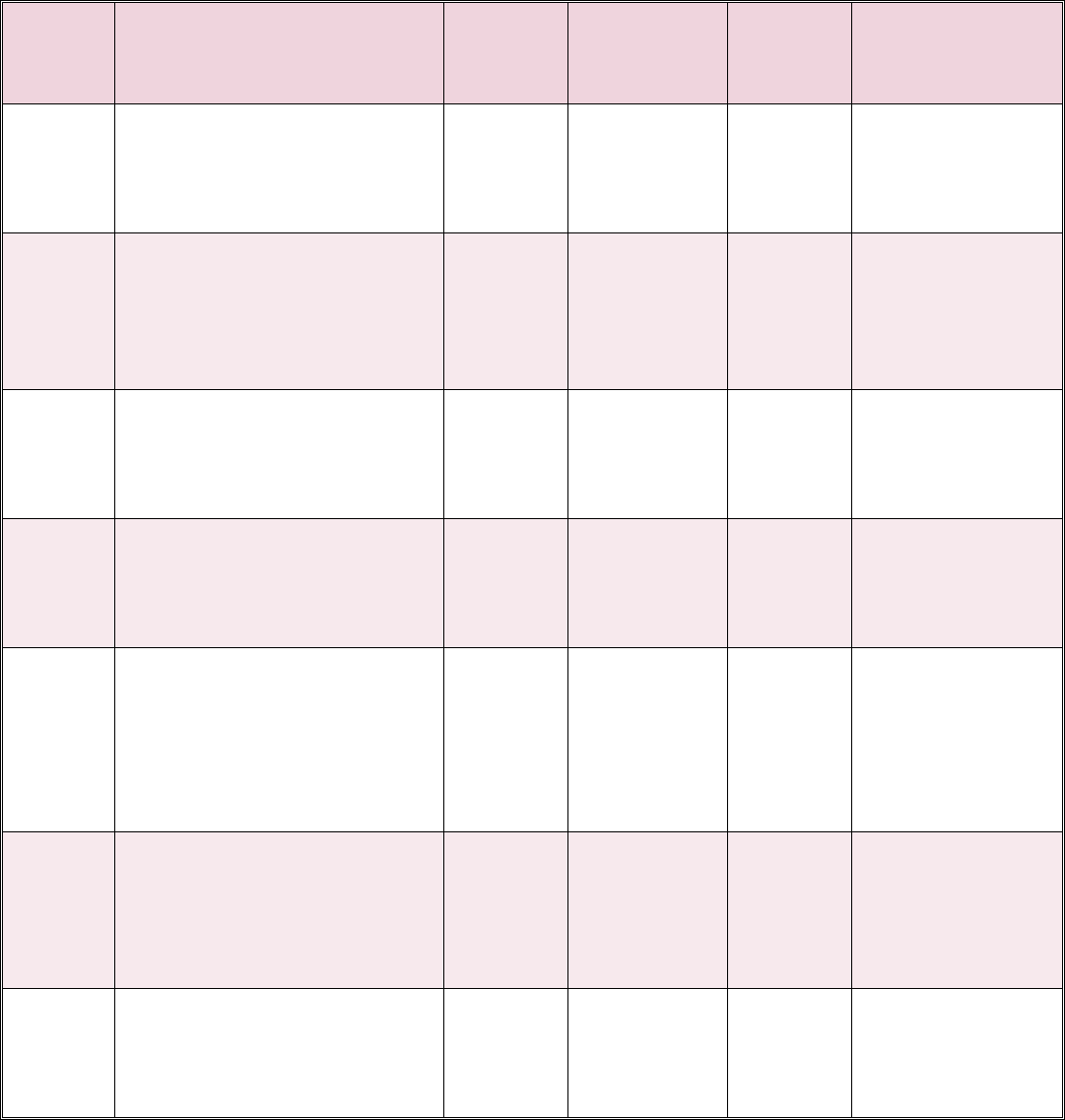
Event
Events that Permit May Self Only to
Change
Time Limits
Code for
Enrollment Changes Enroll Self and
Plans or
SF 2809
Family
Options
3E Reenrollment of former spouse
who voluntarily disenrolls from
May
Reenroll
N/A N/A During open season
a Medicare-sponsored HMO or
Medicaid
3F Former spouse or eligible child
loses FEHB coverage because
Yes Yes Yes From 31 days
before through 60
covering enrollment is
days after date of
terminated, canceled, or
changed to self only
loss of coverage
3G Enrolled former spouse or
N/A Yes Yes From 31 days
eligible child loses coverage
under another group insurance
before through 60
days after date of
plan (but see 3D and 3E)
loss of coverage
3H Former spouse or eligible
family member loses coverage
because FEHB plan is
N/A Yes Yes During open
season, unless
OPM sets a
discontinued in whole or part
different time
3I Former spouse or covered
family member move or take
N/A Yes Yes Upon notifying the
employing office of
job outside the HMO’s service
the move or change
area, or if already outside this
area, move or take job further
of place of
employment
from this area
3J On becoming eligible for
Medicare (You may make this
N/A No Yes At any time
beginning the 30th
change only once in a lifetime.)
day before
becoming eligible
for Medicare
3K Former spouse’s annuity is not
No No Yes Retirement System
enough to make the FEHB
withholdings for plan in which
will advise former
spouse of options
enrolled
34
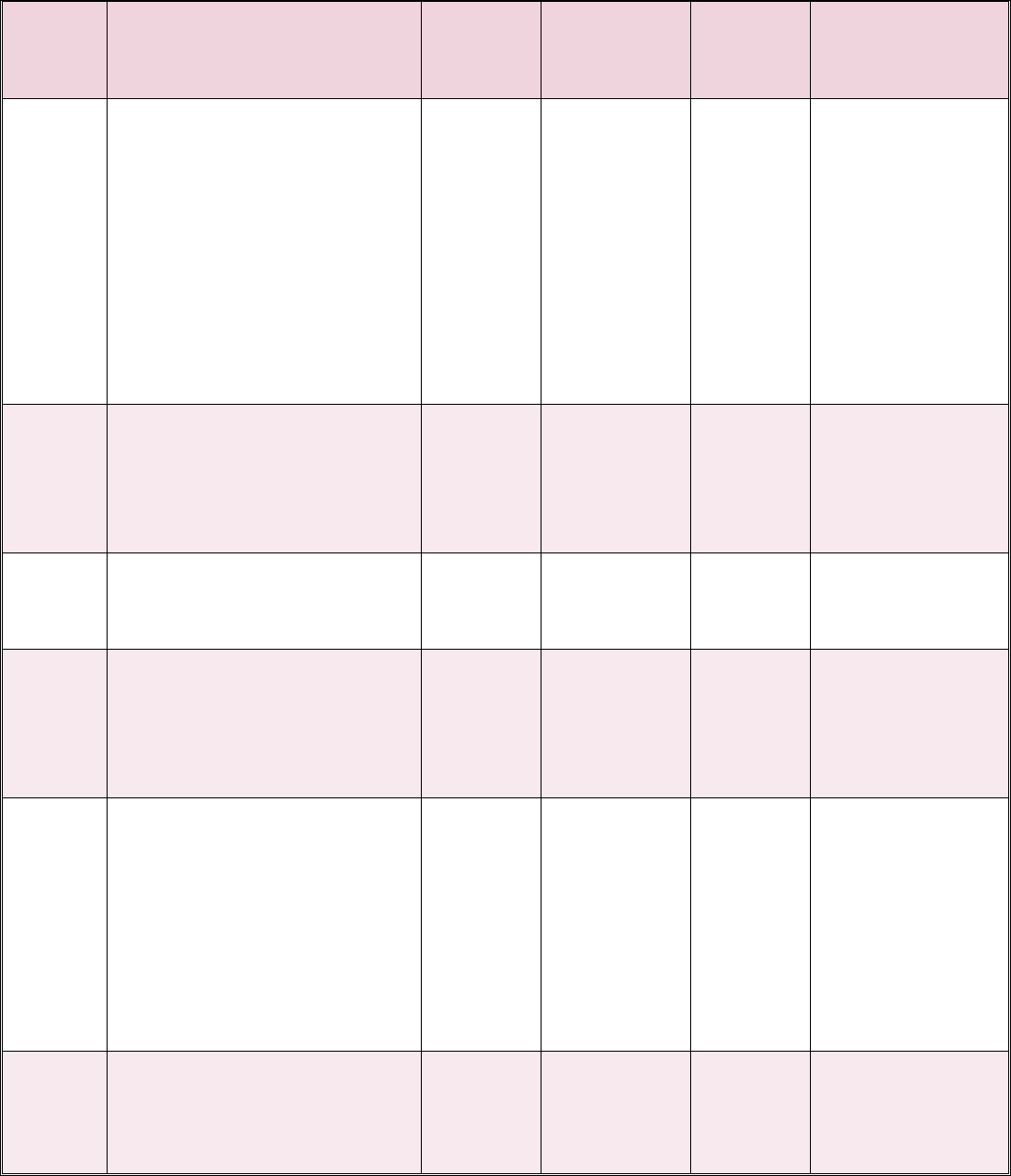
Temporary Continuation of Coverage Enrollees
Event
Code for
SF 2809
Events that Permit
Enrollment Changes
May
Enroll
Self Only to
Self and
Family
Change
Plans or
Options
Time Limits
4A Opportunity to enroll for
continued coverage under
Temporary Continuation of
Coverage (TCC) provisions
Yes Yes, for
former
employee.
N/A for
former spouse
and child who
ceases to
qualify as a
family
member
Yes, for
former
employee.
N/A for
former
spouse and
child who
ceases to
qualify as
a family
member
Within 60 days
after the qualifying
event, or receiving
notice of eligibility,
whichever is later.
4B Open season No Yes* Yes As announced by
the Office of
Personnel
Management
(OPM)
4C Change in family status (except
former spouse)
No Yes Yes From 31 days
before through 60
days after event
4D Change in family status of
former spouse based on addition
of family members who are also
eligible family members of the
employee or annuitant
No Yes Yes From 31 days
before through 60
days after event
4E Reenrollment after Temporary
Continuation of Coverage
(TCC) enrollment terminated
because of other Federal
Employees Health Benefits
(FEHB) coverage; then the other
FEHB coverage is lost before
the TCC eligibility period (18 or
36 months) expires
May
Reenroll
N/A N/A From 31 days
before through 60
days after the
event. Enrollment
is retroactive to the
date of the loss of
the other FEHB
coverage
4F Enrollee or eligible family
member loses coverage under
FEHB or another group
insurance plan (but see 4E)
No Yes Yes From 31 days
before through 60
days after date of
loss of coverage
35
Event
Code for
SF 2809
Events that Permit
Enrollment Changes
May
Enroll
Self Only to
Self and
Family
Change
Plans or
Options
Time Limits
4G Enrollee or eligible family
member loses coverage because
FEHB plan is discontinued in
whole or part
N/A Yes Yes During open
season, unless the
Office of Personnel
Management
(OPM) sets a
different time
4H Enrollee or covered family
member in a Health
Maintenance Organization
(HMO) move or take job outside
the service area, or if already
outside this area, move or take
job further from this area
N/A Yes Yes Upon notifying the
human resources
office of the move
or change of place
of employment
4I On becoming eligible for
Medicare (You may make this
change only once in a lifetime.)
N/A No Yes At any time
beginning on the
30th day before
becoming eligible
for Medicare
* Former spouse may change to self and family only if family members are also eligible family members of
the employee or annuitant.
36

Retirement & Insurance Service
Serving over 10 million customers, Federal employees,
annuitants, and their families.
